More than 19% of American adults (over 40 million people) struggle with anxiety disorders every year.[1] Anxiety disorders are very treatable. Most common anti-anxiety medications like SSRIs and SNRIs are safe to use with Suboxone, but there may be some increased risks of side effects. Benzodiazepines, which are prescribed for panic disorder and panic attacks, may occasionally be prescribed concurrently with Suboxone but with great caution due to overdose risk.
Talk with your doctor about your mental health and opioid use disorder (OUD) and all the medications you take. Together, you can find a combination that helps you stay safe and in remission.
What is Anxiety?
Anxiety is a common mental health disorder characterized by feelings of fear, dread, and uneasiness.[2] People with anxiety frequently have intrusive thoughts or concerns that may cause them to avoid certain situations due to worry.
Anxiety also can cause physical symptoms, such as:[2]
- Dizziness
- Fast heart rate
- Feeling weak or tired
- Rapid breathing
- Sweating
- Trembling
- Trouble concentrating or rapid thoughts
Anxiety is a normal emotion that is experienced by all human beings. However, when anxiety symptoms begin to impair functioning and quality of life, we call this an anxiety “disorder.”
Co-Occurring Anxiety Disorder and Opioid Use Disorder
Generally speaking, people with a substance use disorder are more likely to have a co-occurring mental health disorder and vice versa.[7]
When it comes to opioid use disorder and anxiety disorder, one study found that nearly 30% of people with OUD also had an anxiety disorder.[8]
It’s essential to receive integrated treatment for co-occurring OUD and anxiety because these conditions influence one another. If only the OUD is treated, anxiety symptoms may increase the risk of relapse. And if only the anxiety disorder is treated, it will be difficult to overcome opioid misuse.
Unfortunately over 52% of individuals don’t receive any treatment for addiction or their mental health disorder.[7]
Mixing Suboxone & Benzos
One class of medications that are sometimes used to treat severe anxiety is called benzodiazepines. Benzodiazepines are usually used short-term for severe anxiety, as they have risks including addiction/dependency as well as respiratory depression and sedation.
Benzodiazepines, sometimes referred to simply as “benzos”, include medications such as:
- Clonazepam (Klonopin)
- Lorazepam (Ativan)
- Alprazolam (Xanax)
More than 22% of people with anxiety have been treated with benzodiazepines, and of those people, more than 88% took them for more than 12 weeks. [3]
Many of the 4 million people who take benzodiazepines daily meet the criteria for substance dependence. Taking the drug daily, even for just one month, can lead to distressing withdrawal symptoms. [4]
Because both medications are potentially sedating, they can cause oversedation and respiratory depression. In 2021, 14% of all opioid-involved overdoses also involved benzodiazepines. [5]
In 2021, 14% of all opioid-involved overdoses also involved benzodiazepines. [5]
Benzodiazepines can be taken with Suboxone in appropriate circumstances and under extreme caution, but patients using this strategy should be carefully monitored by a mental health or addiction professional. Taking these medications together should be done slowly and at the lowest doses possible to effectively treat both the OUD and the anxiety disorder.
Overdose Risk
One of the biggest risks of mixing benzodiazepines and Suboxone is profound respiratory depression and overdose. This is because Suboxone, which contains the opioid buprenorphine, and benzodiazepines are both central nervous system (CNS) depressants.
This means they slow down brain functioning, leading to slowed heartbeat and respiratory rate. When combining two CNS depressants, you run the risk of oversedation and dangerously slowed or stopped breathing which can include an overdose.
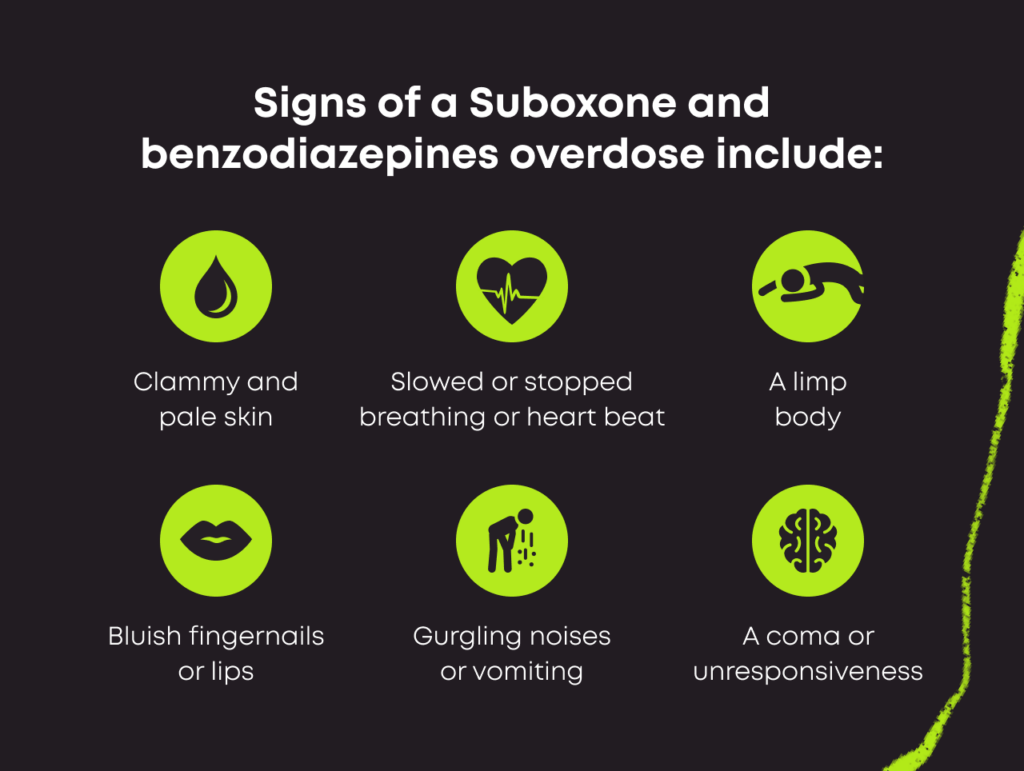
Signs of an overdose on Suboxone and benzodiazepines include:[9]
- Slowed or stopped breathing
- Slowed or stopped heart beat
- Clammy, pale skin
- Limp body
- Blue-ish fingernails or lips
- Gurgling noises
- Vomiting
- Unresponsiveness
- Coma
If you suspect you or someone else has overdosed, call 911 immediately. Administer Narcan (naloxone), if you have it on hand.
What Anxiety Medications Are Safe to Take With Suboxone?
The good news is that first line medications for anxiety are not benzodiazepines and are generally safe to combine with Suboxone.
They are usually several other classes of anxiolytics that are not addictive including:
- Selective serotonin reuptake inhibitors (SSRIs): These medications are commonly prescribed for anxiety and depressive disorders and include Zoloft, Prozac, Lexapro and more.
- Selective serotonin and norepinephrine reuptake inhibitors (SNRIs): These medications are also prescribed for depression and anxiety disorders and include Effexor XR and Cymbalta.
- Tricyclic antidepressants: Among the earliest antidepressants developed, common examples include Elavil, Asendin and Anafranil.
- Norepinephrine-dopamine reuptake inhibitors (NDRIs): Wellbutrin is also prescribed to treat depression and anxiety as well as a host of other conditions.
Talk With Your Doctor
Since certain anti-anxiety medications can have interactions with Suboxone, your doctor should closely monitor you when you initiate anxiolytics and Suboxone together. In general, it is best to try first line options such as SSRIs, SNRIs, or tricyclic antidepressants prior to resorting to benzodiazepines, which have more risks when combined with Suboxone.
If you or someone you know is on Suboxone but also struggling with an anxiety disorder, contact your healthcare provider to discuss your treatment options.

Reviewed By Peter Manza, PhD
Peter Manza, PhD received his BA in Psychology and Biology from the University of Rochester and his PhD in Integrative Neuroscience at Stony Brook University. He is currently working as a research scientist in Washington, DC. His research focuses on the role ... Read More
- Anxiety Disorders: Facts and Statistics. Anxiety and Depression Association of America. https://adaa.org/understanding-anxiety/facts-statistics. Accessed January 2023.
- Anxiety. National Library of Medicine. https://medlineplus.gov/anxiety.html. May 2020. Accessed January 2023.
- Patterns of Benzodiazepines Use in Primary Care Adults with Anxiety Disorders. Heliyon. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6039319/. July 2018. Accessed January 2023.
- Risks Associated with Long-Term Benzodiazepine Use. American Family Physician. https://www.aafp.org/pubs/afp/issues/2013/0815/p224.html. August 2013. Accessed January 2023.
- Benzodiazepines and Opioids. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/opioids/benzodiazepines-opioids. November 2022. Accessed January 2023.
- Benzodiazepines for the Long-Term Treatment of Anxiety Disorders. The Lancet. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)00934-X/fulltext. July 2021. Accessed January 2023.
- Comorbidity: Substance Use and Other Mental Disorders. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/comorbidity/comorbidity-substance-use-other-mental-disorders-infographic. August 2018. Accessed December 2023.
- Santo T Jr, Campbell G, Gisev N, et al. Prevalence of mental disorders among people with opioid use disorder: A systematic review and meta-analysis. Drug Alcohol Depend. 2022;238:109551. doi:10.1016/j.drugalcdep.2022.109551
- Opioid Overdose. Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/opioid-overdose. December 2023. Accessed December 2023.
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Related Content
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.