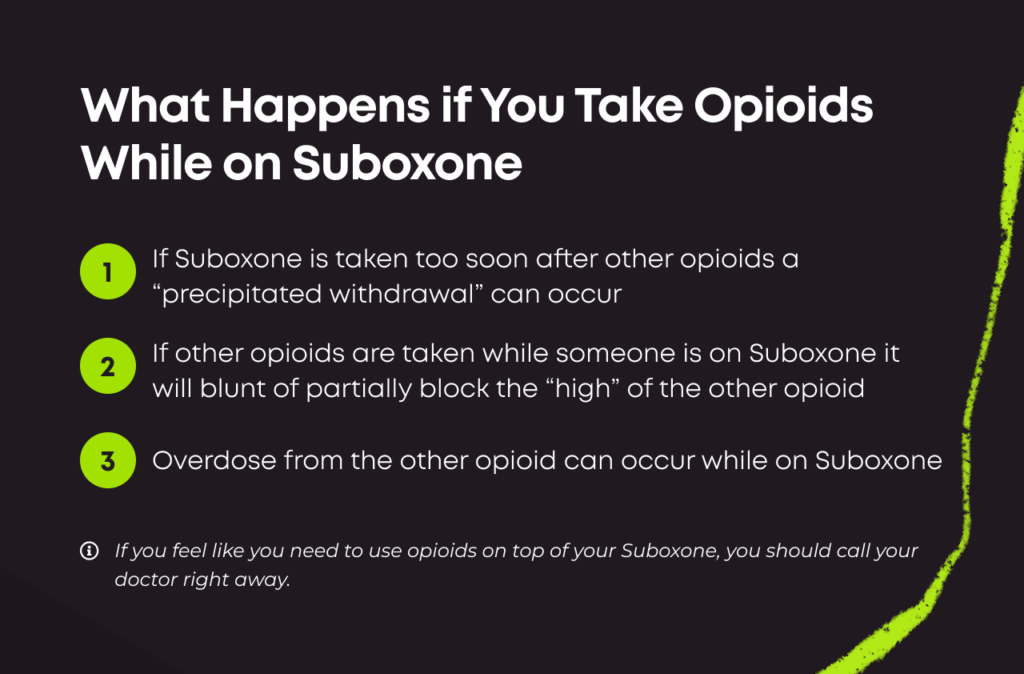
If you take opioids like oxycodone, hydrocodone, heroin, or fentanyl while on Suboxone, you may experience one of two very serious consequences.
- Overdose: Your opioids combine with the buprenorphine in your Suboxone and cause sedation and death.
- Precipitated withdrawal: The buprenorphine in Suboxone binds preferentially to opioid receptors over the opioids in your system, kicking them off quickly and causing a withdrawal syndrome.
While full opioids can be taken along with Suboxone, this should be done with medical supervision to avoid one or the other of these consequences.
The Consequences of Taking Opioids and Suboxone
| First Medication | Second Medication | Consequence |
| Take Suboxone for OUD | Take an opioid at a regular dose | Less intense euphoria or pain relief |
| Take Suboxone for OUD | Take an opioid at higher doses to overcome blocked effects | Increased risk of sedation, respiratory depression, and overdose |
| Take opioid like oxycodone, hydrocodone, or heroin | Take Suboxone shortly after | Precipitated withdrawal symptoms, like nausea, vomiting, diarrhea, anxiety, fever, sweating, muscle aches and more |
The Consequences of Mixing Suboxone & Opioids
Precipitated Withdrawal
If an individual takes a full agonist opioid (such as fentanyl, oxycodone or heroin) and then takes buprenorphine/naloxone (Suboxone) too soon afterward, the buprenorphine (a partial agonist) will bind preferentially over the full opioid and quickly kick the other opioid off the receptors.
This can cause the acute onset of what is known as precipitated withdrawal symptoms. This can feel like a flu-like illness, including symptoms such as the following:
- Headaches
- Chills
- Nausea
- Vomiting
- Diarrhea
- Muscle aches
- Joint pain
- Fever
Precipitated withdrawal typically occurs within about 30 minutes of administering buprenorphine.[3] If you already have Suboxone in your system, the time frame for problems triggered by opioid drugs (like heroin or fentanyl) can depend on how quickly the opioids you use are metabolized.
Precipitated withdrawal symptoms are typically more severe than natural withdrawal symptoms.[3]
Experts say these episodes, while often mild, can be life-threatening in the most severe cases, especially if symptoms like nausea and diarrhea lead to dehydration.[4]
Extremely unpleasant withdrawal can also be a trigger for illicit drug use to relieve these symptoms. Returning to drug use can increase the risk of overdose, as drug tolerance dips.[5] A dose that seems safe could be too much for a healing body to handle.
If you recently used an opioid and want to quit and take Suboxone for your opioid use disorder (OUD), talk to your doctor about how long you should wait before taking your Suboxone dose. You should already be in opioid withdrawal before you take it.
If you experience signs of precipitated withdrawal, contact your doctor immediately. Explain what happened and how you’re feeling. If you can’t reach your doctor, visit an urgent care clinic or hospital instead.
Opioid Overdose
Suboxone binds more strongly to receptors in the brain than full opioids, even though it is less potent. This means that if you take a full opioid like oxycodone after already having Suboxone in your system, you probably won’t get much of the effect of the full opioid, including the “high” or euphoric feelings that opioids produce.
This ability to block other opioids is a protective effect of Suboxone. Some people who relapse while taking Suboxone may misuse high doses of heroin or opioid painkillers in an attempt to overcome these protective effects. And at high doses, especially in combination with buprenorphine, this can lead to an opioid overdose.
An opioid overdose causes the following symptoms:[6]
- Constricted pupils, even in dim light
- Loss of consciousness
- Shallow or slow breathing
- Choking or gurgling sounds
- Pale or blue-tinged skin
If someone is overdosing, follow these steps:[7]
- Call 911 immediately. Stay on the phone and follow instructions until help arrives.
- Administer naloxone per the package instructions.
- Try to keep the person awake and breathing.
- If you can’t wake the person up, turn them on their side to prevent choking.
What if I Need Opioids For Medical Reasons?
Even though you should never take illicit opioids while taking Suboxone, there may be circumstances in which you need prescription opioids for acute pain – for example, after surgery, a dental procedure, an accident, etc.
If you’re taking Suboxone and need surgery, you can receive opioids in addition to your Suboxone. Depending on the situation, your doctor might recommend continuing Suboxone during the procedure versus temporarily stopping Suboxone while you receive opioids and then promptly restarting.
If you need additional pain control, opioids can be given on top of normal Suboxone therapy. However, make sure this is done under medical supervision to avoid either an overdose or precipitated withdrawal. Speak with your doctor before any planned surgical procedures or anticipated need for pain medications, so you and your medical team can have a plan in place for pain management.
Frequently Asked Questions About Taking Opioids and Suboxone
In special circumstances, under strict medical supervision, you can take oxycodone with Suboxone. This is typically only done in the short term to manage severe pain, such as after surgery. If you are taking Suboxone for OUD, you should never take oxycodone without medical supervision.
In most circumstances, you should not be taking oxycodone after you take your Suboxone dose, given that buprenorphine/naloxone is typically prescribed to treat OUD. However, if you are taking it medically and prescribed by a doctor, listen to your provider’s instructions. They may recommend you take your oxycodone several hours after you take your Suboxone to reduce the risk of oversedation.
Yes, Suboxone blocks the effects of fentanyl. This is because Suboxone contains buprenorphine, a partial opioid agonist, and naloxone, an opioid antagonist. Buprenorphine binds to opioid receptors and kicks fentanyl off them. Naloxone, being an opioid antagonist, also blocks fentanyl at the receptor site.
Yes, under a doctor’s supervision, you can take hydrocodone while taking Suboxone. Typically, hydrocodone is only prescribed for a short period of time to manage severe pain. If this is the case, make sure you follow your physician’s instructions very carefully in order to reduce the risk of harmful side effects or interactions.

Reviewed By Peter Manza, PhD
Peter Manza, PhD received his BA in Psychology and Biology from the University of Rochester and his PhD in Integrative Neuroscience at Stony Brook University. He is currently working as a research scientist in Washington, DC. His research focuses on the role ... Read More
- Emergency Department Buprenorphine/Naloxone (Suboxone): Home Dosing Information. Government of Alberta. https://myhealth.alberta.ca/health/AfterCareInformation/pages/conditions.aspx?hwid=custom.ab_suboxone_homedosing_ac_adult. March 2021. Accessed September 2022.
- Buprenorphine. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK459126/. May 2022. Accessed September 2022.
- A Case of Buprenorphine-Precipitated Withdrawal Managed with High-Dose Buprenorphine. Family Practice. https://academic.oup.com/fampra/article/39/2/292/6309967. April 2022. Accessed January 2024.
- Opioid Withdrawal. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK526012/. July 2023. Accessed January 2024.
- Association Between Mortality Rates and Medication and Residential Treatment After Inpatient Medically Managed Opioid Withdrawal: A Cohort Analysis. Addiction. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7854020/. February 2020. Accessed January 2024.
- Preventing Opioid Overdose. Centers for Disease Control and Prevention. https://www.cdc.gov/opioids/overdoseprevention/index.html. October 2021. Accessed January 2024.
- Opioid Overdose. U.S. Department of Veterans Affairs. https://www.mentalhealth.va.gov/substance-use/overdose.asp. Accessed January 2024.
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Related Content
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.