Xanax is a benzodiazepine medication that has the potential for misuse, dependence, and addiction. Several Xanax alternatives exist for anxiety and panic disorder if an individual is concerned about this misuse potential or has otherwise struggled with addiction in the past and wants to avoid potentially addictive substances. These non-addictive anxiety medications include drugs belonging to the class of selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) as well as buspirone, hydroxyzine, and beta-blockers.
How Xanax Works
Alprazolam, known by the brand name Xanax, is an anti-anxiety drug that belongs to the class of benzodiazepines.[1] Benzodiazepines act on gamma-aminobutyric acid (GABA) neurotransmitters to produce a relaxing anti-anxiety effect.
For this reason, Xanax is often taken to treat sudden-onset symptoms or short-term anxiety. Other commonly prescribed drugs of this class include diazepam (Valium), lorazepam (Ativan), clonazepam (Klonopin), temazepam (Restoril), chlordiazepoxide (Librium), and midazolam (Versed).
Xanax’s Misuse Potential
When taken properly and treatment does not extend beyond a few weeks, the addiction potential for Xanax is relatively low. However, when taking benzodiazepines more often or for longer than intended or by misusing Xanax, the risk for addiction as well as tolerance and physical dependence increases.[2]
Long-term side effects of Xanax use include the following:[1]
- Loss of coordination
- Disinhibition
- New or worsening depression or anxiety
- Suicide thoughts
- Cognitive impairment
- Increased risk of dementia
- Psychosis
- Drowsiness
- Nausea or vomiting
- Delirium
Additionally, withdrawal from Xanax comes with serious side effects. Physical dependence can begin within a few days of taking the drug, even when taking it as prescribed, depending on the individual and their proclivity to develop physical dependence.
Xanax Withdrawal Symptoms
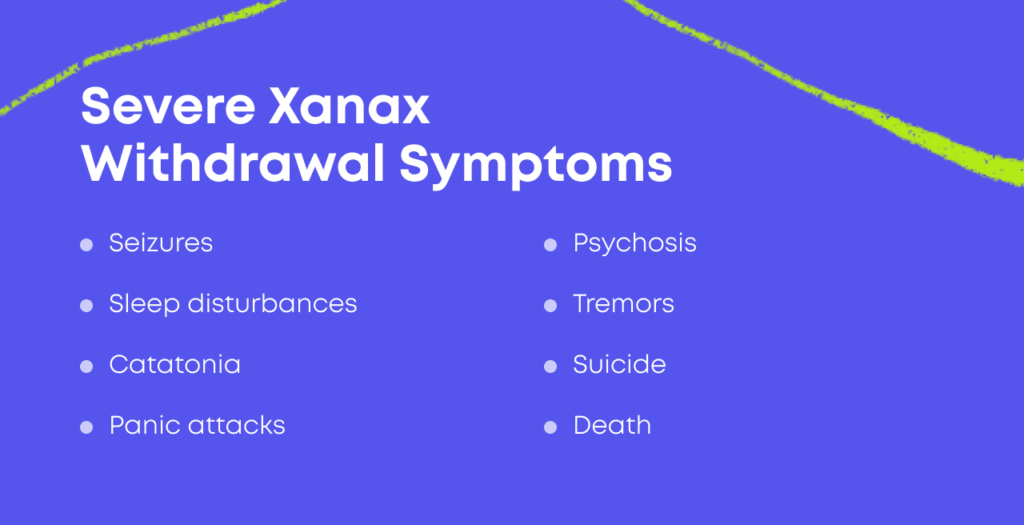
The symptoms of Xanax withdrawal can be severe, especially when stopping the drug abruptly.[3] Quitting after prolonged use can be dangerous, with withdrawal lasting weeks to months.
Severe withdrawal symptoms can resemble acute alcohol withdrawal and may include the following:[1],[3]
- Seizures
- Sleep disturbances
- Catatonia
- Panic attacks
- Psychosis
- Tremors
- Suicide
- Death
Discontinuing the use of long-term benzodiazepines like Xanax should happen under the supervision of a doctor. Although medical detox cannot prevent withdrawal symptoms, specialists can help reduce the severity of symptoms, alleviate discomfort, and develop a treatment plan.
Most importantly, working with a doctor to develop a plan to stop taking benzodiazepines helps protect a person from the most dangerous withdrawal symptoms, allowing them to be addressed before they become life-threatening.
Non-Addictive Alternatives to Xanax
While benzodiazepines are still commonly prescribed for anxiety disorders, there are better options that are generally safer, with a lower risk of addiction. Many of these medications can be used on a long-term basis, although it is important to talk to your doctor about the potential benefits and downsides of each option and ask about any long-term health effects a treatment option may have.
Here are some of the non-addictive alternatives to Xanax you could try:
- SSRIs
For many prescribers, the non-addictive drugs of choice to treat anxiety disorders are selective serotonin reuptake inhibitors (SSRIs). SSRIs have lower misuse potential and fewer long-term side effects associated with their use. SSRIs are considered one of the first-line treatments for chronic anxiety disorders.
SSRIs block the recycling of the neurotransmitter serotonin back into cells, thus leaving higher amounts of it available to act on the brain.[4] Serotonin regulates mood, digestion, sleep, libido, and more. Drug alternatives in this class used to treat anxiety disorders include:
- Prozac (fluoxetine)
- Zoloft (sertraline)
- Citalopram (Celexa)
- Lexapro (escitalopram)
SSRIs take around four to eight weeks to take effect and may produce side effects like headache, nausea, trouble sleeping, and dizziness. However, in the majority of people, side effects are mild and disappear after the first few days, and the treatment benefits outweigh the issues.
- SNRIs
Like SSRIs, serotonin and norepinephrine reuptake inhibitors (SNRIs) have a lower risk of misuse, dependence, and addiction.
In addition to increasing serotonin levels, SNRIs also block the recycling of norepinephrine, increasing levels of this vital brain chemical.
These drugs are typically used if first-line medications like Prozac or Lexapro fail to control or help alleviate anxiety. SNRIs include:
- Effexor (venlafaxine)
- Cymbalta (duloxetine)
- Pristiq (desvenlafaxine)
- Buspirone
Buspirone is a unique non-benzodiazepine anxiolytic originally used as an antipsychotic but found to better treat generalized anxiety disorder (GAD).[6] It may be used in place of or alongside SSRIs to mitigate unfavorable side effects.
- Hydroxyzine
Hydroxyzine is an antihistamine drug in the class of allergy medications but also has some sedating and anxiolytic effects.
It has little to no addiction potential but does help to take as needed for short-term, severe anxiety, and thus might be a good alternative for someone who does not want to become dependent on benzodiazepines.
- Beta Blockers
Beta-blockers are typically taken to treat hypertension (high blood pressure).[7] However, they are also sometimes used to treat the physical symptoms of anxiety, such as shaking or sweating. Two commonly prescribed beta-blockers for this off-label use are atenolol and propranolol.
These drugs work by acting on two key messenger chemicals in the body, adrenaline and noradrenaline. When the body gets anxious, these chemical messengers cause certain unwanted side effects, such as sweating, shaking, and elevated heart rate. Beta-blockers block the effects of these chemical messengers, reducing the physical symptoms of anxiety and partially helping with psychological symptoms as well.
While these drugs aren’t habit-forming, it usually isn’t recommended that a person take them on a long-term basis. They don’t generally cause harm even with months or years of use, but regular checkups can help make sure they aren’t impacting your health. Notably, a person should get their blood pressure checked more regularly when using beta blockers.
Ways to Manage Anxiety at Home
Typically, the best way to manage anxiety is with a combination of strategies, such as medication, therapy, self-care practices, and coping strategies you can engage in at home. Some coping strategies and self-care practices for anxiety include:
- Meditation and mindfulness
- Yoga
- Journaling about anxiety and panic attacks
- Practice deep breathing techniques
- Develop and practice grounding techniques, such as naming one thing you can hear, touch, taste, smell, and see
- Listen to relaxing music
- Take a bath
- Talk to someone you trust
- Go on a walk
If you find that you are unable to manage your anxiety with a combination of therapy and self-care practices, you may need medication to help reduce your symptoms and improve functioning. When you talk to your doctor, make sure to disclose any history of substance use disorder or drug misuse.

Reviewed By Peter Manza, PhD
Peter Manza, PhD received his BA in Psychology and Biology from the University of Rochester and his PhD in Integrative Neuroscience at Stony Brook University. He is currently working as a research scientist in Washington, DC. His research focuses on the role ... Read More
- Alprazolam. National Library of Medicine. https://medlineplus.gov/druginfo/meds/a684001.html. May 2021. Accessed September 2022.
- 1 in 4 Older Adults Prescribed a Benzodiazepine Goes on to Risky Long-Term Use, Study Finds. Institute for Healthcare Policy & Innovation. https://ihpi.umich.edu/news/1-4-older-adults-prescribed-benzodiazepine-goes-risky-long-term-use-study-finds. September 2018. Accessed September 2022.
- Benzodiazepine Withdrawal. Emergency Medicine News. https://journals.lww.com/em-news/fulltext/2001/12000/benzodiazepine_withdrawal__potentially_fatal,.13.aspx. December 2001. Accessed September 2022.
- Fluoxetine. National Library of Medicine. https://medlineplus.gov/druginfo/meds/a689006.html. January 2022. Accessed September 2022.
- Venlafaxine. National Library of Medicine. https://medlineplus.gov/druginfo/meds/a694020.html. January 2022. Accessed September 2022.
- Repurposing Buspirone for Drug Addiction Treatment. International Journal of Neuropsychopharmacology. https://academic.oup.com/ijnp/article/16/2/251/623187. October 2012. Accessed September 2022.
- Propranolol. NHS UK. https://www.nhs.uk/medicines/propranolol/. November 2021. Accessed September 2022.
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Related articles
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.