Benzodiazepines are medications used acutely for alcohol withdrawal, either in the hospital or at certain inpatient detox facilities. Currently, benzodiazepines are considered the “gold standard” medication for acute alcohol withdrawal, able to relieve symptoms, prevent complications like delirium tremens and keep someone safe during detox. [1]
What Medication is Used for Alcohol Withdrawal?
Quick Answer
Benzodiazepines like diazepam, lorazepam and chlordiazepoxide are the best and safest medications for managing acute alcohol withdrawal symptoms. Alcohol and benzodiazepines are cross-tolerant and have similar mechanisms of action, which is why benzodiazepines are so effective at mitigating alcohol withdrawal symptoms.
What are Benzodiazepines?
Benzodiazepines or benzos are a class of depressant medications prescribed to manage insomnia, anxiety, panic disorders, seizures and muscle spasms.
They are also used to manage and treat acute alcohol withdrawal—this is because they can relieve symptoms, reduce the risk of complications like seizures and delirium tremens and decrease cravings. [1]
Alcohol Withdrawal Symptoms Benzos Can Treat
Benzodiazepines have a similar mechanism of action as alcohol, which means they are highly effective at relieving alcohol withdrawal symptoms, such as:[2]
- Anxiety
- Panic attacks
- Hand tremor
- Shakiness
- Sweating
- Rapid pulse
- Nausea and vomiting
- Hallucinations or psychosis
- Seizures
Benzodiazepines are especially effective at reducing the risk of severe alcohol withdrawal, known as delirium tremens, as well as grand mal seizures.[1]
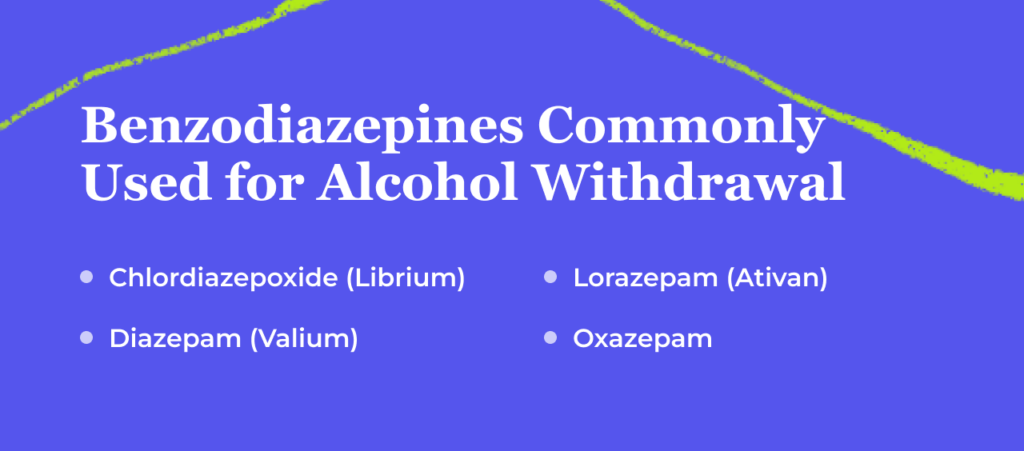
Which Benzodiazepines Are Used for Alcohol Withdrawal Treatment?
Many benzodiazepines are suitable choices for alcohol withdrawal treatment, with the goal generally being an option that works quickly and is long-lasting. Common choices include the following:[1]
- Chlordiazepoxide (Librium)
- Diazepam (Valium)
- Lorazepam (Ativan)
- Oxazepam
These benzodiazepines are the best-studied medications for alcohol withdrawal, although other drugs in this class may be used as well.[1] Generally, long-acting benzos with larger half-lives are better because they need to be administered less frequently, which is why Xanax, a short-acting medication, is usually not the first choice. Also, short-acting benzos have a greater chance of rebound symptoms of withdrawal.[1]
Lorazepam is often given to patients who have liver issues, elderly patients, or those with lung conditions that may be affected by severe sedation.[1]
How Are Benzodiazepines Given During Alcohol Detox?
Benzodiazepines may not be necessary for mild alcohol withdrawal symptoms. They are more commonly used when a patient has a history of complicated or severe withdrawal or they have severe alcohol use disorder. Benzos are usually administered in an inpatient setting, such as in the hospital, for patients undergoing acute alcohol withdrawal. Benzodiazepines are usually given orally but can also be administered intravenously for severe and rapid symptom relief.
Benzodiazepines can typically be given in one of three ways when treating withdrawal.
Symptom-Triggered Regimen (STR)
The first is through what is called a symptom-triggered regimen (STR) where a person’s withdrawal symptoms are rated via a scale, and drug doses are administered based on withdrawal severity.[1],[3] This is typically the preferred treatment method as it involves the least use of medication and doctors don’t run the risk of over-sedation.
- Only used in inpatient settings
- Is best done under medical supervision
- Suitable for mild to severe alcohol withdrawal symptoms
- Dose is based on the patient’s self-reporting
Fixed Tapering Dose Regimen (FTDR)
Another option is a fixed tapering dose regimen (FTDR), where a patient receives fixed doses of benzodiazepine on a predetermined schedule, tapering off them over time. This method is helpful when a patient can’t be monitored as closely by a trained professional or when they may be unable or unwilling to rate their withdrawal symptoms on a scale.[1]
- Best for an outpatient setting
- Dose isn’t individualized or tailored
- Works for mild symptoms
Sample Benzos Schedule
Generally, the benzodiazepine dose for a fixed tapering dose regimen depends on the person’s average daily alcohol intake.[4]
| Benzo | Dose | Frequency |
| Lorazepam | 2mg | Every 6 hours for 4 doses then |
| 1mg | Every 6 hours for 8 doses | |
| Oxazepam | 30mg | Every 6 hours for 4 doses then |
| 15mg | Every 6 hours for 8 doses | |
| Diazepam | 10mg | Every 6 hours for 4 doses then |
| 5mg | Every 6 hours for 8 doses | |
| Chlordiazepoxide | 50mg | Every 6 hours for 4 doses then |
| 25mg | Every 6 hours for 8 doses |
Loading Dose Regimen (LDR)
The last option is what is called a loading dose regimen (LDR), where long-acting benzodiazepines are given in high doses immediately, usually in the case of someone with a history of severe alcohol withdrawal in anticipation of another complicated withdrawal. This method requires very close monitoring and may require admission to the intensive care unit (ICU). [1]
- Best for people at risk of severe withdrawal / delirium tremens
- Only used in a hospital that allows monitoring
- Best way to prevent seizures
Benefits of Benzodiazepines for Alcohol Withdrawal
There are many advantages of using benzodiazepines to manage alcohol withdrawal, including: [1]
- They help patients achieve medical stabilization
- They help provide a humane and safe detox environment
- They can prevent delirium tremens, agitation and seizures, which can be life-threatening otherwise
- There are many benzodiazepines to choose from, enabling tailored treatment
- They are generally well-tolerated
- Make it easier to go through alcohol withdrawal and then transition into alcohol rehab
- They have a wide margin of safety
- They have a low risk of dependence and tolerance when used short-term
Medical Detox: The Safest Setting for Alcohol Withdrawal
If you have an alcohol use disorder and need help quitting drinking, a medical detox setting is considered the safest environment. Medical detox can occur in a number of settings, including:
- Psychiatric hospital
- Acute care unit
- Freestanding detox center that offers medical care
- Inpatient rehab that offers medical care
What matters most is that there is a team of doctors and nurses available to provide you with 24/7 supervision and monitoring to ensure your safety and comfort.
Aside from administering benzodiazepines to manage alcohol withdrawal and reduce your risk, the medical team will also provide:
- Monitoring of your vital signs
- Supportive care like IV fluids
- Additional medications, if needed, such as anticonvulsants
- Detox counseling
- Case management
Dos & Don’ts of Benzo Use for Alcohol Withdrawal
Do Keep Hopeful
Many people who struggle with alcohol misuse may have attempted to quit in the past. Alcohol withdrawal can be an intensely uncomfortable and even potentially dangerous experience. However, with proper medical supervision, alcohol withdrawal is safe and doable. Alcohol withdrawal usually lasts for no longer than one week. After that, your symptoms should greatly improve—especially with the use of benzos. [2]
Do See a Doctor
Getting through alcohol withdrawal on your own can be very difficult and even dangerous in the case of severe withdrawal.
If you are attempting to discontinue alcohol use and you have a history of complicated alcohol withdrawal, severe AUD, medical or mental health problems, poor liver functioning, brain lesions or older age, make sure you talk to your doctor about medical detox and benzodiazepine use—this can help save your life. Whatever you do, never attempt to quit drinking cold turkey. This can have life-threatening consequences. It may be appropriate and safer for you to be admitted to the hospital or to another medical facility so you can undergo detox under medical supervision.
Don’t Self-Prescribe
You should never take someone else’s prescription medication or purchase benzodiazepines illicitly in order to self-treat alcohol withdrawal. Instead, you should always talk to your doctor about the safest way to go through withdrawal. Medications can be prescribed for support.
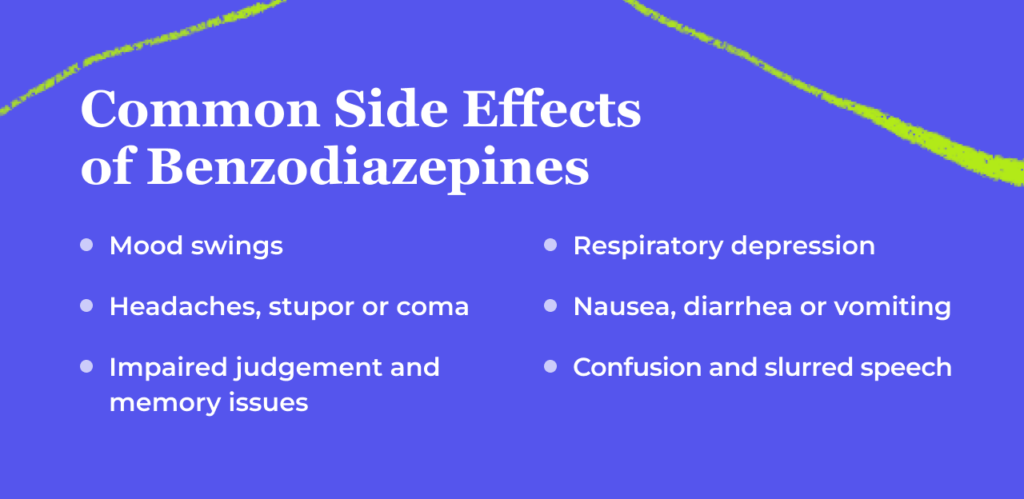
Risks of Benzodiazepines
Benzodiazepines are controlled substances that have risks of their own. They can cause respiratory depression and therefore must be given carefully, particularly in patients with other medical conditions such as COPD, cardiovascular problems, or dementia.
In particular, these risks increase if given concurrently with other sedating medications, such as opioids. For example, In 2021, 14% of overdose deaths related to opioids also involved benzodiazepines.[6]
Benzodiazepines also have addiction potential. The rate of benzodiazepine misuse among people using the drugs is fairly low compared to other substances such as opioids, however, the risk is still there: Of about 30.5 million American users, an estimated 17.1% engaged in what could be considered misuse of their benzodiazepine prescription. Fewer than 2% developed what would be considered a benzodiazepine use disorder. [7]
Some side effects of benzos to be aware of include: [2],[8]
- Mood swings
- Impaired judgment
- Slurred speech
- Coordination problems
- Cognitive and memory issues
- Stupor or coma
- Respiratory depression
- Confusion
- Headache
- Nausea or vomiting
- Diarrhea
- Tremors
However, because benzodiazepines and alcohol are cross-tolerant, someone with AUD or severe alcohol dependence and tolerance may not experience such intense side effects of the medication.
When you enter the hospital or a detox center, the medical team will conduct a thorough evaluation in order to determine the best course of treatment for you—this includes which benzodiazepine will be best for your needs as well as any other medications or treatment modalities necessary. And they will monitor you around the clock so they can make any adjustments as needed.
Frequently Asked Questions About Benzos for Alcohol Withdrawal
No, benzodiazepines are not considered medication for addiction treatment (MAT) for alcohol use disorder (AUD), but rather, they are used short-term for alcohol withdrawal and detox. There are, however, several FDA-approved medications for alcohol use disorder to help prevent cravings and relapse. These medications include naltrexone (Vivitrol), disulfiram (Antabuse) and acamprosate (Campral).
Doctors usually administer benzodiazepines like lorazepam, diazepam, oxazepam and chlordiazepoxide for the management of acute alcohol withdrawal.
Benzodiazepines are used to treat alcohol withdrawal because they have a similar mechanism of action as alcohol, meaning they are cross-tolerant. They have been proven to be effective and safe for the management of this condition and can help prevent life-threatening symptoms like seizures and delirium tremens.[5]

Reviewed By Peter Manza, PhD
Peter Manza, PhD received his BA in Psychology and Biology from the University of Rochester and his PhD in Integrative Neuroscience at Stony Brook University. He is currently working as a research scientist in Washington, DC. His research focuses on the role ... Read More
- Alcohol Withdrawal Syndrome: Benzodiazepines and Beyond. Journal of Clinical & Diagnostic Research. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4606320/. September 2015. Accessed August 2022.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
- Symptom-Triggered Therapy for Alcohol Withdrawal Syndrome: A Systematic Review and Meta-Analysis of Randomised Clinical Trials. Journal of General Internal Medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6544709/. June 2019. Accessed August 2022.
- Clinical management of alcohol withdrawal: A systematic review. Ind Psychiatry J. 2013;22(2):100-108. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085800/. Accessed August 2023.
- Alcohol withdrawal syndrome. Am Fam Physician. 2004;69(6):1443-1450. https://www.aafp.org/pubs/afp/issues/2004/0315/p1443.html. Accessed August 2023.
- Benzodiazepines and Opioids. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/opioids/benzodiazepines-opioids. April 2022. Accessed August 2022.
- Research Suggests Benzodiazepine Use Is High While Use Disorder Rates Are Low. National Institute on Drug Abuse. https://nida.nih.gov/news-events/science-highlight/research-suggests-benzodiazepine-use-high-while-use-disorder-rates-are-low. October 2018. Accessed August 2022.
- Benzodiazepines. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing https://www.ncbi.nlm.nih.gov/books/NBK470159/. January 2023. Accessed August 2023.
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Related articles
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.