Snorting Suboxone is dangerous. Ingredients inside Suboxone tablets aren’t made to connect with nasal tissues. Sniffing them can lead to burning, stinging, and tingling sensations, microvascular tears, nasal bleeding, infection, tissue damage, etc.
In addition, snorting Suboxone can also cause precipitated withdrawal, which means you’ll immediately go into opioid withdrawal.
If you’re tempted to misuse your Suboxone by snorting it or otherwise, talk to your treatment team. Your overall treatment plan may need some adjustment to ensure you stay on track.
Can You Snort Suboxone?
Quick Answer
No, you should never snort Suboxone (buprenorphine/naloxone). Snorting Suboxone is considered misuse and can cause severe nasal damage and other health risks. Additionally, if you sniff Suboxone, you won’t get high—you will go into precipitated withdrawal, which includes uncomfortable flu-like symptoms.
What Is Suboxone?
Suboxone is the brand name for a combination of a partial opioid agonist, buprenorphine, and an opioid receptor blocker, naloxone.[1] Suboxone is prescribed to treat opioid use disorder (OUD) and works by alleviating cravings and withdrawal symptoms.[1],[2]
Adding naloxone to buprenorphine reduces the risk that people will misuse Suboxone by taking it in ways that are not prescribed, such as by snorting it. When the medication is not taken sublingually — for example, when it is snorted —naloxone prevents the buprenorphine from binding to opioid receptors and protects against an overdose. [3]
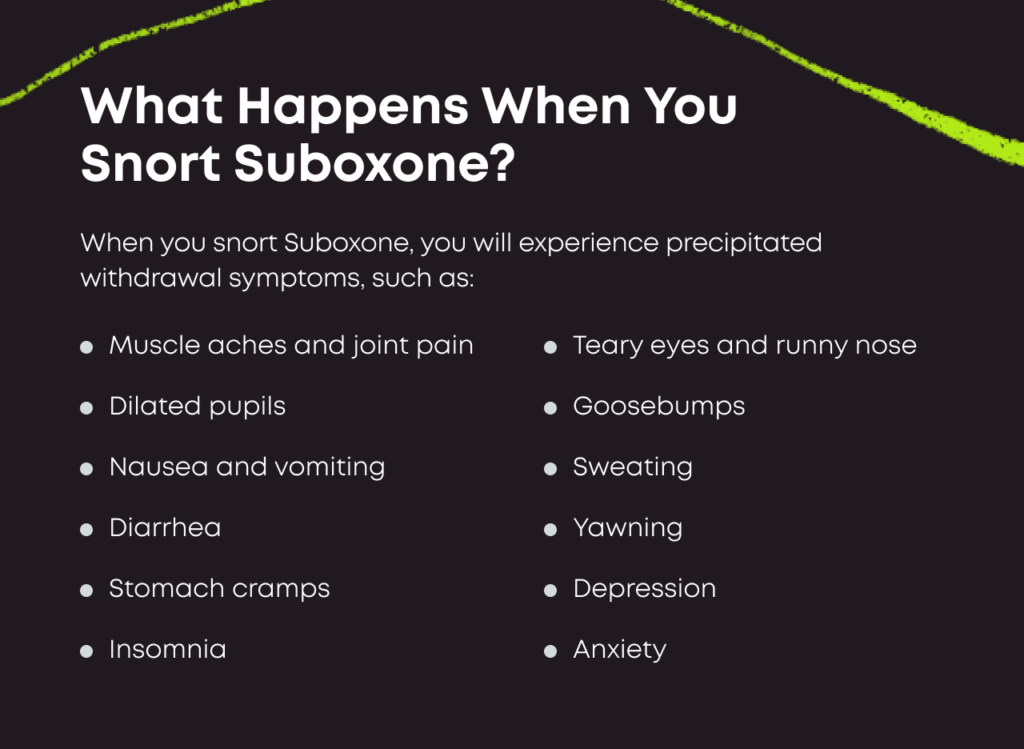
What Happens When You Snort Suboxone?
When a person snorts Suboxone, they won’t experience the high they are looking for. Instead, the naloxone component will become activated and cause you to go into precipitated withdrawal. [3]
Precipitated withdrawal is the same as opioid withdrawal and involves symptoms, such as:[4]
- Nausea and vomiting
- Diarrhea
- Sweating
- Fever
- Goosebumps
- Stomach cramps
- Muscle aches and bone pain
- Profound yawning
- Anxiety
- Agitation
- Runny nose and teary eyes
These symptoms can last anywhere from a few hours to a couple days, depending on many factor
Does Snorting Suboxone Get You High?
Snorting Suboxone won’t usually get you high. If snorted, the naloxone component of buprenorphine will kick in and block the therapeutic effects of buprenorphine. Sniffing Suboxone or any other buprenorphine/naloxone medication will cause you to go into immediate opioid withdrawal.
This is designed to prevent people from attempting to misuse Suboxone by snorting or injecting it.
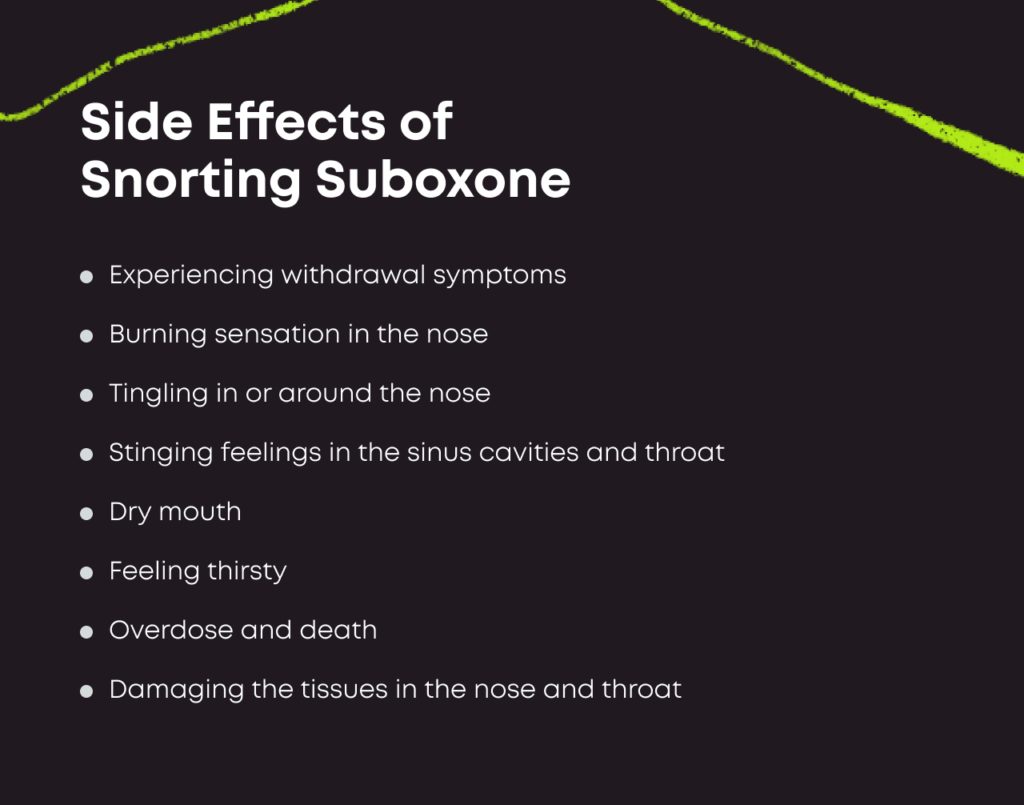
Other Side Effects of Snorting Suboxone
Snorting Suboxone can not only make you feel sick and precipitate withdrawal—it can also cause many harmful side effects to your health.
Side effects of Suboxone snorting include the following:[2]
- Burning sensations in your nose
- Tingling in or around your nose
- Stinging sinuses
- Dry mouth
- Microvascular tears
- Nasal bleeding
- Sinusitis
- Infection
- Tissue damage
- Perforated nasal septum
Some people develop infections from snorting Suboxone, especially if they use unclean tools to crush or inhale their drugs.
Snorting High Doses of Suboxone Can Lead to Overdose
While Suboxone contains anti-overdose ingredients, snorting extremely high doses in an attempt to overcome buprenorphine’s ceiling effect can lead to overdose. So can combining Suboxone with other depressants like benzodiazepines or alcohol.
Suboxone overdose symptoms include the following:[1]
- Pinpoint pupils
- Slow or stopped breathing
- Slow or stopped heartbeat
- Unresponsiveness
- Gurgling noises
- Blue-ish lips or fingernails
- Unconsciousness
If you suspect someone has overdosed, call 911 immediately and stay by their side.
What Are the Long-Term Dangers of Snorting Suboxone?
Of all the long-term risks associated with snorting Suboxone, recurring opioid use disorder (OUD) is the most severe.
You’re taking Suboxone to address an OUD that has harmed your health, your family and your future. Misusing that medication means your OUD is still present and that it’s not effectively managed. You could move from snorting Suboxone to snorting or injecting other opioids like heroin in time.
Continued snorting of any drug, including Suboxone, can lead to severe tissue damage within your nose, sinuses and throat. If the damage is extensive, you could need surgery to fix the effects.
About Suboxone Misuse
Suboxone is formulated so that its misuse potential is low. Though it is still technically possible to misuse this substance, euphoric effects are minimal, especially in people who are using other opioids at high doses and are tolerant.
Other medications used to treat opioid use disorder have more misuse potential than Suboxone. For example, methadone, a full opioid agonist, has a much higher misuse potential than Suboxone. Because of the Naloxone component of Suboxone, it is less likely to be misused than buprenorphine alone. [7]
The Benefits of Suboxone Treatment
Suboxone is extremely important for the millions of people in the United States seeking to overcome problems with substance use. In 2018, more people died from opioid overdoses than from the peaks of HIV, gun violence, or car accidents. [8]
Suboxone has been a game-changer in preventing relapse to opioid use. Peer-reviewed studies consistently show that medications for opioid use disorder, especially Suboxone, reduce relapse rates and improve long-term recovery rates.[9,10]
Suboxone treatment is increasingly available as a prescription outpatient option through telemedicine services like Bicycle Health.
Treatment for Suboxone Misuse
If you’re misusing your addiction treatment medications, talk to your team. You may need additional therapy to keep your substance use disorder under control, or you might benefit from a different type of medication.
If you don’t have a prescription for Suboxone and you’re misusing it, talk to your doctor about treatment. Buying Suboxone from dealers isn’t safe. A comprehensive treatment program that combines medications and therapy could be what you need to get your life back on track.

Reviewed By Peter Manza, PhD
Peter Manza, PhD received his BA in Psychology and Biology from the University of Rochester and his PhD in Integrative Neuroscience at Stony Brook University. He is currently working as a research scientist in Washington, DC. His research focuses on the role ... Read More
- Buprenorphine/Naloxone (Suboxone). National Alliance on Mental Illness (NAMI). https://www.nami.org/About-Mental-Illness/Treatments/Mental-Health-Medications/Types-of-Medication/Buprenorphine/Buprenorphine-Naloxone-(Suboxone). January 2021. Accessed December 2021.
- Buprenorphine. Substance Abuse and Mental Health Services Administration (SAMHSA). https://www.samhsa.gov/medication-assisted-treatment/medications-counseling-related-conditions/buprenorphine. May 2021. Accessed December 2021.
- Intelligence Bulletin: Buprenorphine: Potential for Abuse. National Drug Intelligence Center. https://www.justice.gov/archive/ndic/pubs10/10123/10123t.htm. September 2004. Accessed December 2021.
- Opiate and Opioid Withdrawal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/000949.htm. May 2020. Accessed December 2023.
- Tompkins CN, Wright NM, Waterman MG, Sheard L. Exploring prison buprenorphine misuse in the United Kingdom: a qualitative study of former prisoners. Int J Prison Health. 2009;5(2):71-87. doi:10.1080/17449200902880482.
- Determination That SUBUTEX (Buprenorphine Hydrochloride) Sublingual Tablets, Equivalent 2 Milligrams Base and Equivalent 8 Milligrams Base, Were Not Withdrawn from Sale for Reasons of Safety or Effectiveness. Federal Register. https://www.federalregister.gov/documents/2015/02/13/2015-03001/determination-that-subutex-buprenorphine-hydrochloride-sublingual-tablets-equivalent-2-milligrams. February 2015. Accessed December 2021.
- Jones JD, Sullivan MA, Vosburg SK, et al. Abuse potential of intranasal buprenorphine versus buprenorphine/naloxone in buprenorphine-maintained heroin users. Addict Biol. 2015;20(4):784-798. doi:10.1111/adb.12163.
- Velander JR. Suboxone: Rationale, Science, Misconceptions. Ochsner J. 2018;18(1):23-29. PMID: 29559865.
- Connery, Hilary Smith. Medication-Assisted Treatment of Opioid Use Disorder: Review of the Evidence and Future Directions. Harvard Review of Psychiatry. https://journals.lww.com/hrpjournal/FullText/2015/03000/Medication_Assisted_Treatment_of_Opioid_Use.2.aspx?casa_token=EpvYkcA4kRQAAAAA:qQLteHzO2f6joZKS9HdlJpSWz_G2BRdGoIG1zKeVnyPLFW_EsDaHqVWb_ZM0Qwa-2RKy6dideGZkv6gt5t8uFp2vl6Y. March/April 2015. Accessed January 2022.
- Walsh, Sharon L.; Nuzzo, Paul A.; Babalonis, Shanna; Casselton, Victoria; Lofwall, Michelle R. Intranasal Buprenorphine Alone and in Combination With Naloxone: Abuse Liability and Reinforcing Efficacy in Physically Dependent Opioid Users. Drug and Alcohol Dependence. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4833536/. May 2016. Accessed January 2022.
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Related Content
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.
