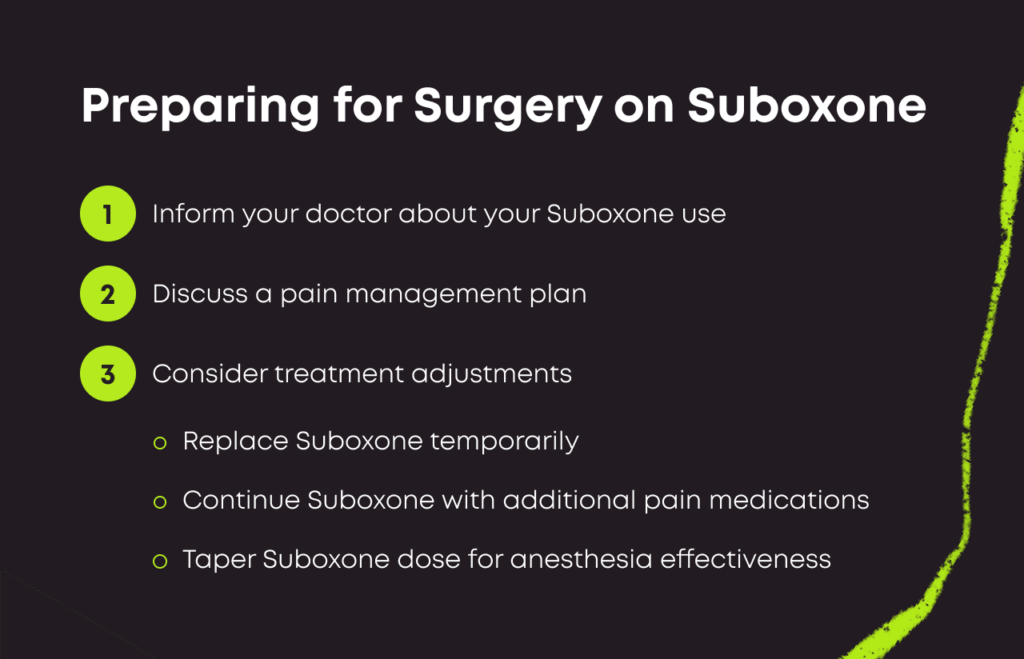
You should tell your doctor prior to any planned surgery that you are on Suboxone use before your surgery. The medication can interfere with common techniques used in operating rooms, and you may need special considerations to help manage your pain after surgery.
Suboxone & Surgery: What You Should Know
Suboxone is both a medication to help treat OUD as well as manage pain. It has analgesic properties and helps relieve pain to a certain degree. However, during and after surgery you may have increased pain control needs, and therefore it is very smart to talk to your surgeon and post operative team ahead of any planned surgery so that you can discuss a plan for your pain management. Depending on your specific case, your doctor may decide to stop Suboxone temporarily, or to continue it but give you additional pain medications after your procedure.
During anesthesia, doctors typically provide high doses of opioids to produce unconsciousness. Suboxone could keep those therapies from working as they might in a sober patient. Therefore it is important to tell your doctor ahead of time that you are on Suboxone so that together, you can come up with a plan for your care both intra-operatively and post-operatively.
Your doctor may recommend the following:
- Replacing: Swapping out Suboxone for another opioid could remove your cravings without blocking more drugs from latching.[1]
- Staying: Your risk of relapse is high if you stop Suboxone. To lower that risk, some doctors recommend that their patients keep taking doses as planned with no changes. They make a surgery plan with this situation in mind.[2]
- Tapering: Your team may decide that now is a good time to lower your Suboxone dose. A smaller amount could allow the anesthesia to move smoothly without increasing relapse risks. This requires careful management by your treatment team.
As you determine what to do with your Suboxone dose, your medical team can consider how to keep you comfortable on the operating table. They might do the following:[3]
- Increase: Your team might give you a very large amount of opioids that can overpower your Suboxone dose.
- Alter: Your team could use local anesthetics to lower your pain and allow for smaller general anesthesia doses.
- Monitor: Your team should also watch your breathing carefully, as large opioid doses can slow down your inhales and exhales.
Every surgery is different, and medical teams often have complex flow charts and rules that help them decide what is best for their patients.[4] Be as open and honest as you can during your surgery planning process so the team can work with you.
Emergency Surgeries: What You Should Know
If you require an urgent surgery and ou don’t have time to alter your Suboxone, it can be a tricky situation.
Your team has three basic approaches, depending on the level of your anticipated postoperative pain:[5]
- Mild: They might continue your buprenorphine dose as usual.
- Moderate: They might continue your Suboxone and add additional pain medications, even opioids, in addition to your regular Suboxone
- High: They might temporarily stop your Suboxone and start opioid medications with a plan to restart Suboxone promptly either at the end of your hospitalization or immediately upon leaving the hospital
Make sure you advocate for yourself! Because Suboxone is a relatively new medication, a lot of surgeons may not be familiar with how best to manage pain in patients on Suboxone. They may incorrectly believe that because you are already on Suboxone, your pain should be controlled without additional medications. This is not usually true. In addition, they may not feel comfortable prescribing you additional pain medications for fear that they will interact with your Suboxone. This is also a mistake – many pain medications can be given along with Suboxone without stopping the Suboxone, safely.
Ask your Suboxone prescriber – either a primary care doctor, a pain management specialist, a psychiatrist, etc – to contact your surgeon directly so they can advise the surgeon about how best to manage your pain needs for any upcoming surgery.
- Pain Management in Patients Taking Suboxone. Outpatient Surgery. https://www.aorn.org/outpatient-surgery/articles/outpatient-surgery-magazine/2009/march/anesthesia-alert. March 2009. Accessed April 2022.
- Surgery, Buprenorphine, and Patients in Recovery from Opioid Use Disorder. American Society of Regional Anesthesia and Pain Medicine. https://www.newswise.com/articles/surgery-buprenorphine-and-patients-in-recovery-from-opioid-use-disorder. September 2021. Accessed April 2022.
- Perioperative Management of a Patient Taking Suboxone at the Time of Ambulatory Surgery. Case Reports in Anesthesiology. https://www.hindawi.com/journals/cria/2020/5628348/. 2020. Accessed April 2022.
- UCSF Guideline for the Perioperative Management of Buprenorphine. University of California San Francisco. https://www.fresno.ucsf.edu/wp-content/uploads/2021/06/UCSF-Perioperative-Management.pdf. January 2018. Accessed April 2022.
- Buprenorphine and Surgery: What's the Protocol? Practical Pain Management. https://www.practicalpainmanagement.com/resource-centers/opioid-monitoring-2nd-ed/buprenorphine-surgery-what-protocol. April 2019. Accessed April 2022.
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Related Content
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.