Both opioid use disorder (OUD) and alcohol use disorder (AUD) can be treated with medication-assisted treatment (MAT).
The prescription drugs used in medication-assisted treatment (MAT) are evidence-based therapies.[1] People who use MAT are NOT substituting one medication for another”. Instead, they are addressing both the physical and psychological components of substance misuse.
MAT therapies are used for alcohol use disorders (AUD) and opioid use disorders (OUD). While the basic concepts remain the same, the specifics differ. Let’s dive into those differences.
MAT for Alcohol
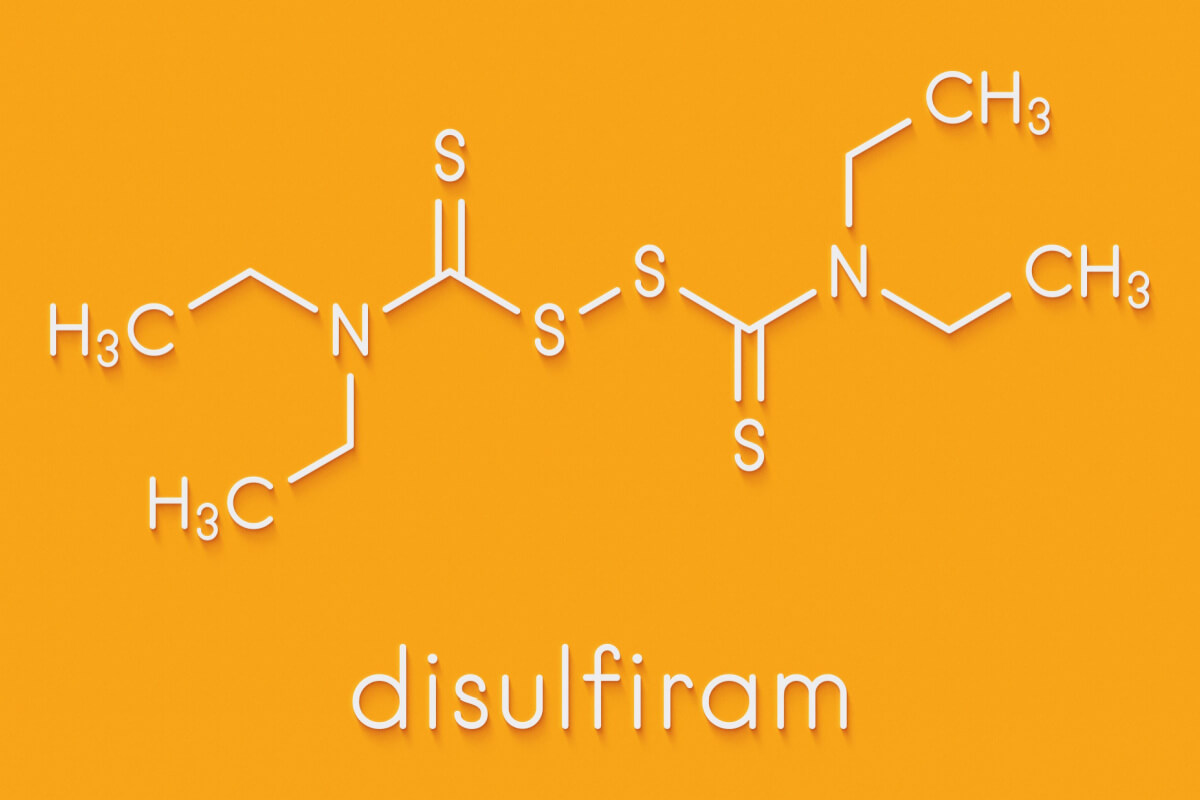
AUD is defined as the continued use of alcohol, even when it harms your life, health, or both. There are several MAT for AUD, including acamprosate, disulfiram, and naltrexone.
Specialists recognize three common MAT options:
- Disulfiram: This medication is one of the older medications used for alcohol cessation. However, due to the side effects of causing nausea and vomiting, it has generally fallen out of favor as a treatment for alcohol use disorder. However, some patients who have been on it for years may continue to use it comfortably.
- Acamprosate: Acamprosate is a medication usually given 3 times a day to help prevent cravings for alcohol. It is particularly safe for patients who may have concurrent liver disease as a result of their drinking.
- Naltrexone: Naltrexone is the most efficacious and most commonly used medication for AUD these days. It has few side effects and is well tolerated. It is generally given once a day at a dose of either 50 or 100 mg. It is safe to use with most medications except for opioid medications, as it is an opioid blocker. Thus, if a patient is taking opioid medications, they should not take Naltrexone simultaneously because it can induce a withdrawal syndrome.
Experts aren’t sure how long MAT for AUD should last. Some say the treatment is most effective when it lasts for at least six months and up to a year.[2] However, if a patient feels that MAT for OUD is helpful, it is likely safe for them to continue medications for a much longer period of time, potentially indefinitely, to prevent relapse. Talk to your doctor about long term use of MAT for AUD.
MAT for Opioids
OUD is defined as the continued use of opioid medications despite negative physical or social consequences.
MAT can be life saving to help people resist urges to use opioids. There are 3 main MAT for OUD: Buprenorphine, methadone and naltrexone.
Methadone
Methadone is a full opioid agonist. Currently in the US, it is dispensed only through certified methadone clinics. This partial agonist also blunts withdrawal symptoms and eases cravings. If you do relapse, it will be less rewarding.
Your methadone clinic will dispense a daily dose usually in a liquid form. Depending on your clinic, you will likely have to come to clinic daily, at least at first, to receive your medication. Once stable, some clinics do offer “take home doses” so that you do not have to come on a daily basis. Methadone is a highly efficacious medication for preventing OUD relapse. doses will be in a liquid you take each day, and typically, you must go to a clinic to get the medication.
Buprenorphine
Buprenorphine, also called by its brand name “Suboxone”partial opioid agonist, meaning that it gives the patient a certain amount of opioid to prevent withdrawal cravings, but without enough “agonism” to make you high or allow you to become so sedated or intoxicated that you are at risk of overdose. Most formulations of buprenorphine come in strips or tablets that are dissolved under the tongue, however there are other methods of administration as well depending on your needs, including injectable, patches, or implants. Buprenorphine can be prescribed by a licensed provider at a clinic a month at a time which in many ways makes it logistically easier for patients than attending a daily methadone clinic.
Naltrexone
Naltrexone is a third MAT for OUD. It is also used for AUD. Naltrexone works mechanistically very differently from Buprenorphine and Methadone, which are opioid agonists. Naltrexone works the opposite way: It is an opioid antagonist, meaning it blocks the effects of opioids. This means that if a patient takes naltrexone and then takes an opioid, the effects of that opioid will be blocked and the patient will not be able to get high or accidentally overdose. While this medication many be helpful to prevent opioid overdose, it does not prevent opioid withdrawal cravings in the same way that buprenorphine or methadone do, and thus may not be as successful a treatment for patients that are going through acute withdrawal from opioids. However, some patients do find it to be a helpful medication chronically for prevention of opioid misuse particularly after the acute withdrawal phase. It may also be a good alternative option for patients who cannot tolerate buprenorphine or methadone for any number of reasons.
Which Treatment for OUD is Best?
No studies indicate which treatment is best for all people universally.[3] Buprenorphine and methadone are both opioid agonists that treat the unpleasant symptoms of acute withdrawal and cravings and thus they may be preferable over Naloxone short term for OUD. However, Naloxone may be a better option for patients who prefer not to use an opioid medication long term once their acute withdrawal has resolved.
Your doctor will talk with you about your individual goals, where you live, your history of substance misuse, and more to help make the right choice of MAT for you.
How MAT Therapies for AUD and OUD Differ in Terms of Duration
Both forms of MAT, whether they are for alcohol or opioids, involve taking a prescription medication. But the way you take the therapies, how long you need them, and more can differ.
MAT for alcohol use disorder is, in some cases, designed for temporary use. Most patients who use MAT for OUD do so more acutely (for the first 6 months to a year after stopping drinking).
MAT for opioids, on the other hand, is often designed for long-term use. Opioids like heroin and prescription painkillers can cause long-term changes in brain chemistry that can persist throughout the lifespan. You may need medication to ease those changes forever, even when you have been through therapy and changed habits that support recurring drug use.
Medication-Assisted Treatment Success Rates
In one study of MAT for OUDs, researchers followed people for 3.5 years after therapy started. At this point, 61% were abstinent, and fewer than 10% were considered still dependent on opioids.[5]
Studies of AUDs are harder to conduct. They often end early, and the results are never published.[6] But in small studies, researchers find that people who get MAT for alcohol tend to stay sober compared to those that get a placebo.[7]
MAT Comparison Table

By Elena Hill, MD, MPH
Elena Hill, MD; MPH received her MD and Masters of Public Health degrees at Tufts Medical School and completed her family medicine residency at Boston Medical Center. She is currently an attending physician at Bronxcare Health Systems in the Bronx, NY where ... Read More
- MAT Medications, Counseling, and Related Conditions. Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/medication-assisted-treatment/medications-counseling-related-conditions. March 2022. Accessed April 2022.
- Medication for the Treatment of Alcohol Use Disorder: A Brief Guide. Substance Abuse and Mental Health Services Administration. https://store.samhsa.gov/sites/default/files/d7/priv/sma15-4907.pdf. 2015. Accessed April 2022.
- Medications for Opioid Use Disorder. Substance Abuse and Mental Health Services Administration. https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PEP21-02-01-002.pdf. 2021. Accessed April 2022.
- Use of Pharmacotherapies in the Treatment of Alcohol Use Disorders and Opioid Dependence in Primary Care. BioMed Research International. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4299453/. January 2015. Accessed April 2022.
- Long-Term Follow-Up of Medication-Assisted Treatment for Addiction to Pain Relievers Yields Cause for Optimism. National Institute on Drug Abuse. https://archives.drugabuse.gov/news-events/nida-notes/2015/11/long-term-follow-up-medication-assisted-treatment-addiction-to-pain-relievers-yields-cause-optimism. November 2015. Accessed April 2022.
- Rates of Discontinuation and Non-Publication of Trails for the Pharmacologic Treatment of Alcohol Use Disorder. Substance Abuse Journal. https://www.tandfonline.com/doi/abs/10.1080/08897077.2021.2010261. February 2022. Accessed April 2022.
- Pharmacological Interventions for Alcohol Misuse in Correctional Settings: A systematic Review. Alcoholism Clinical and Experimental Research. https://onlinelibrary.wiley.com/doi/abs/10.1111/acer.14751. November 2021. Accessed April 2022.
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Related articles
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.