Precipitated withdrawal can happen if an opioid detox is not overseen by a trained medical professional. It is an experience that can push some people back into active opioid misuse.
Withdrawal symptoms are uncomfortable no matter how they unfold, but with precipitated withdrawal, the symptoms are rapid, severe and exceptionally difficult to navigate.[1]
The good news is that precipitated withdrawal is preventable. Below, you’ll find a step-by-step guide to help you stop this from happening to you or your loved one. With the right information, you can have conversations with your medical team, so you don’t have to worry about it happening accidentally.
Understanding Precipitated Withdrawal
No one living with a dependence on opioids can go straight from active misuse as part of an opioid use disorder (OUD) to abstinence without experiencing withdrawal symptoms. To stop this from happening, patients in medicated detox are given a regimen of medications on a specific timeline to reduce the chances of experiencing withdrawal symptoms.[2]
However, if these medications are not taken correctly, it can cause a sudden, abrupt onset of withdrawal symptoms that are mentally and physically severe, unlike regular opioid withdrawal, in which symptoms build slowly over time. In fact, precipitated withdrawal can occur within minutes, and the symptoms are far more severe.
Symptoms of Precipitated Withdrawal
Symptoms of precipitated withdrawal are the same as regular opioid withdrawal but they come on more intensely and quickly. They may include the following:[1]
- Nausea and vomiting
- Stomach cramps and diarrhea
- Anxiety, agitation and restlessness
- Muscle and bone pain
- Heavy sweating
- High heart rate and blood pressure
- Goosebumps
Common Causes & Risks Factors
The primary cause of precipitated withdrawal is taking an opioid antagonist before all opioids are out of the system.
Drugs like naloxone and naltrexone are common opioid antagonists and may be administered alone (during an opioid overdose) to trigger immediate withdrawal on purpose. Buprenorphine-based medications, including Suboxone, can also trigger precipitated withdrawal if administered too soon in the detox process. This is because buprenorphine, though it binds imperfectly to receptors and does not cause the ‘high’ that potent opioids like fentanyl do, has a higher ‘affinity’ for mu opioid receptors. This means that if a person takes buprenorphine too quickly after using a drug like fentanyl, the buprenorphine will kick the fentanyl off the receptors quickly, displacing it, and sending the person quickly into precipitated withdrawal.
Similarly, in cases where people attempt anesthesia-assisted rapid opioid detox with the goal of expediting the detox process, the process can unfold too quickly and inadvertently trigger precipitated withdrawal.[3]
Recognizing Precipitated Withdrawal
Precipitated withdrawal is almost impossible to miss. Unlike traditional opioid withdrawal, precipitated withdrawal does not come on slowly, starting with mild symptoms that grow in intensity over a period of a few days. It comes on within minutes of taking an opioid antagonist. It is characterized by severe sweating, cramping, diarrhea, vomiting and more.[1]
Take Immediate Action
If you suspect that you are experiencing precipitated withdrawal, seek immediate medical assistance. Especially if you are living with co-occurring medical or mental health disorders, it can be dangerous to undergo precipitated withdrawal without medical support.
Prevention Strategies for Precipitated Opioid Withdrawal
Precipitated opioid withdrawal is not a foregone conclusion. It is possible to prevent it with a well-thought out plan and medical supervision. Here are some tips:
Safe Tapering Techniques
For many, the easiest way to avoid triggering a precipitated opioid withdrawal is to taper off drugs. Don’t quit taking your opioid of choice all at once. Also, avoid taking opioid antagonists. Instead, taper off your dose, taking incrementally less and less over time to avoid an onslaught of withdrawal symptoms.[4]
Though this is likely to trigger a low level of opioid withdrawal symptoms, it will never be as severe as precipitated withdrawal. To do this safely and effectively, it is important to only undertake tapering under the supervision of a medical professional.
Medication Timing
If choosing to use medications like Suboxone (a combination of buprenorphine and naloxone), it is important to get the timing right.
In many cases, a low dose of buprenorphine is prescribed during the initial phase of detox.
When the physician presiding over the detox determines that opioid levels are low enough to introduce the next phase, they will increase the dose. As long as this doesn’t happen until opioid levels are low (when the time is right), the individual should avoid precipitated withdrawal.
Again, the best way to ensure that medication timing is executed appropriately is to only undergo opioid detox under the care of a trained medical professional and never alone. When done effectively, medicated opioid detox saves lives.[5]
FAQs: Common User Questions
These are some of the questions we hear most about precipitated opioid withdrawal:
Precipitated withdrawal will last for varying amounts of time for each person. Individual factors impact the process, including the following:
– The dose of the opiate drug they are taking at the time they enter detox
– The use of other illicit substances (if any)
– The existence of co-occurring or underlying medical and mental health issues
– Whether or not there is a medical professional present to assist with the management of opioid withdrawal symptoms
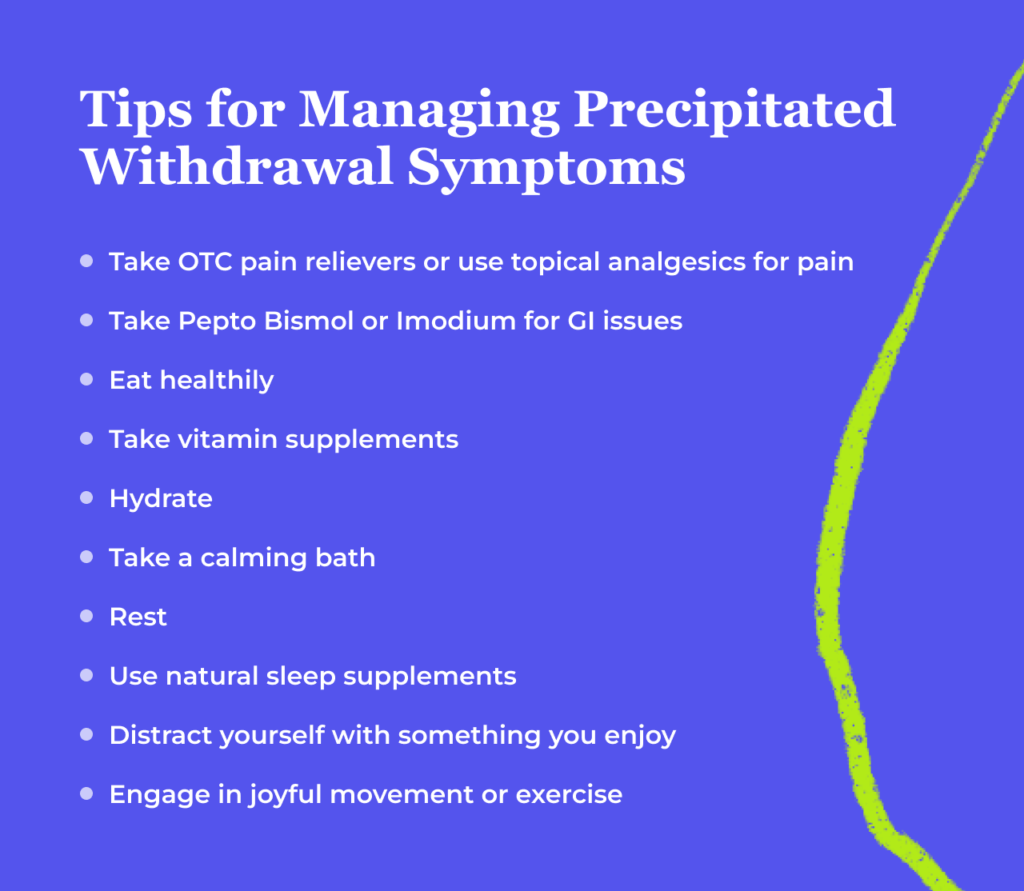
You cannot prevent an issue that you are already experiencing, but you can get treatment to manage it. If you have accidentally entered precipitated withdrawal by taking an opioid antagonist on your own, seek immediate medical care.
If you are undergoing a medicated detox and experience precipitated withdrawal as a result of the treatment, contact your doctor immediately.
Naloxone and naltrexone can both trigger precipitated withdrawal. In some cases, naloxone is used to purposely trigger a precipitated withdrawal in the event of an opioid overdose.[6]
However, it is also an ingredient in the opioid detox treatment medication Suboxone. It is included to help patients avoid relapse if they misuse Suboxone by injecting it.[7] Knowing that taking an opioid in this way will trigger precipitated withdrawal can be helpful in discouraging opioid misuse.
Get Help
Preventing precipitated withdrawal from occurring is as simple as working together with a medical team to ensure that you taper down your dose of opioids slowly enough to avoid an onslaught of symptoms. When you take the time needed to get levels low enough in the system before taking an opioid antagonist and avoid stopping all drug and medication use cold turkey, you can safely detox without risking experiencing a precipitated withdrawal.
Work together with a medical team and stay under the supervision of a doctor while undergoing opioid detox and treatment for OUD. Don’t attempt to go it alone. With the right support, you can stay safe and comfortable.

Reviewed By Peter Manza, PhD
Peter Manza, PhD received his BA in Psychology and Biology from the University of Rochester and his PhD in Integrative Neuroscience at Stony Brook University. He is currently working as a research scientist in Washington, DC. His research focuses on the role ... Read More
- Dunn KE, H. Elizabeth Bird, Bergeria CL, Ware OD, Strain EC, Huhn AS. Operational definition of precipitated opioid withdrawal. 2023;14. https://doi.org/10.3389/fpsyt.2023.1141980
- Information about medication-assisted treatment. U.S. Food and Drug Administration. Published May 23, 2023. Accessed February 12, 2023. https://www.fda.gov/drugs/information-drug-class/information-about-medication-assisted-treatment-mat
- Deaths and severe adverse events associated with anesthesia-assisted rapid opioid detoxification. Centers for Disease Control and Prevention. Accessed February 12, 2023. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6238a1.htm
- Kuntz JL, Dickerson JF, Schneider JL, et al. Factors associated with opioid-tapering success: A mixed methods study. Journal of the American Pharmacists Association. 2021;61(3):248-257.e1. https://doi.org/10.1016/j.japh.2020.12.019
- Mancher M, Leshner AI. The Effectiveness of Medication-Based Treatment for Opioid Use Disorder. National Academies Press (US); 2019. https://www.ncbi.nlm.nih.gov/books/NBK541393/
- Naloxone. Substance Abuse and Mental Health Services Administration. Published September 18, 2023. Accessed February 12, 2023. https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/naloxone
- Opheim A, Gaulen Z, Solli KK, et al. Risk of relapse among opioid‐dependent patients treated with extended‐release naltrexone or buprenorphine‐naloxone: A randomized clinical trial. The American Journal on Addictions. 2021;30(5):453-460. https://doi.org/10.1111/ajad.13151
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Related Content
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.
