You can switch from methadone to Suboxone with the help of your treatment team. How easy it is to make the switch will depend on many factors, including your current methadone dose.
If you’re thinking of switching from methadone to Suboxone for your Medication for Addiction Treatment (MAT), talk to your doctor first. Explain why you believe Suboxone is a better choice for managing your opioid use disorder, and if your doctor agrees, develop a plan together to transition from one to another.
Regardless of whether you wind up switching or not, never stop taking your OUD medications without talking to your treatment team first. If your doctor agrees that Suboxone is a better fit, you may need several office visits to initiate the transition and follow up.
Why Switch from Methadone to Suboxone?
Methadone and Suboxone are both treatments for OUD.
Methadone is the oldest Medication for Addiction Treatment. Doctors started using methadone to treat patients in 1964. Buprenorphine (Suboxone) was later approved by the FDA in 2002.[1]
Even though methadone is an old and proven MAT option, some disadvantages to using methadone over Suboxone might prompt people to consider switching.
Reasons People Switch from Methadone
There are many reasons people may switch from methadone to Suboxone, such as: [2]
- People on methadone face stigma, with more than 30% of people on methadone experiencing hurtful comments from loved ones
- Methadone can only be dispensed out of a methadone clinic, which requires frequent (usually daily) visits and can be a huge burden to people’s quality of life
- Going to the clinic may be a barrier to receiving ongoing methadone, especially for those who are working, attending school, and have other responsibilities
Now that Suboxone is widely available and equally effective at treating OUD in most patients, more patients who have been on methadone in the past are interested in transitioning to Suboxone.
Methadone vs. Suboxone
The table can help you understand the differences between methadone and Suboxone:[9]
| Methadone | Suboxone |
| Induction must be done in a clinic | Induction can be done at home |
| Maintenance doses can potentially be available for at-home use | Maintenance doses are always available for at-home use |
| Visiting a clinic can come with stigma | At-home use can reduce stigma |
| Full opioid agonist | Partial opioid agonist |
| No overdose protections | Ceiling effect and misuse preventive added |
| Moderate withdrawal symptoms | Mild withdrawal symptoms |
| 24-36 hour half-life | 36–48 hour half-life |
| More effective for severe opioid use disorder | Effective for mild/moderate opioid use disorder |
| Oral liquid or tablet | Strip or tablet |
6 Benefits of Switching From Methadone to Suboxone
Opioids were involved in more than 80,000 overdose deaths in 2021 alone.[3] Fortunately, seeking treatment for OUD with the help of methadone or Suboxone can save your life. While either medication can be highly beneficial, some people may prefer one over the other. Here are six reasons you might consider moving from methadone to Suboxone.
Here are some of the reasons you might switch and enjoy the benefits of Suboxone:
1. Fewer Office Visits
In the United States, methadone is only available in methadone centers or clinics.[4] People using this medication must visit their providers often (usually daily). While some people may be eligible for “takeaway/take-home” doses for a few days at a time, most patients still must visit the clinic multiple times a week, which can be a big time and logistical burden.
When comparing Suboxone vs. methadone, access to Suboxone is different. People can use this medication at home without visiting treatment centers regularly. For some people, particularly anyone who must work or who has other daily responsibilities that make daily methadone clinic visits prohibitive, this freedom is essential.
2. Fewer Side Effects
While both Suboxone and methadone attach to opioid receptors, Suboxone’s connection is less potent, which means it may be less likely to cause side effects.
As a result, people often feel less sedated while taking Suboxone compared to methadone.[5] They also may experience milder or fewer side effects than methadone, such as constipation, nausea or dizziness.
3. Health Benefits
Some people with certain cardiac problems, such as “prolonged QT syndrome,” may not take methadone safely.[5] Their doctors might recommend a switch to Suboxone.
4. Lower Risk of Misuse
Misusing methadone is possible, especially if the drug is available for at-home use. Suboxone has a lower risk of misuse. Buprenorphine’s ceiling effect means that, at a certain point, the drug does not become significantly more potent even as the dose increases.
And the naloxone in each dose starts working when people misuse the drug. Due to its lower misuse potential, Suboxone is available for at-home use.
5. Reduced Cravings
Both methadone and Suboxone can ease chemical imbalances caused by opioids like heroin. But if you don’t get relief from methadone, the buprenorphine in Suboxone could be a better option for you.
6. Reduced Stress
You can use Suboxone at home on a schedule that works for you. Making appointments, as you must do for methadone, is not required. You can attend to your everyday life while addressing your OUD.
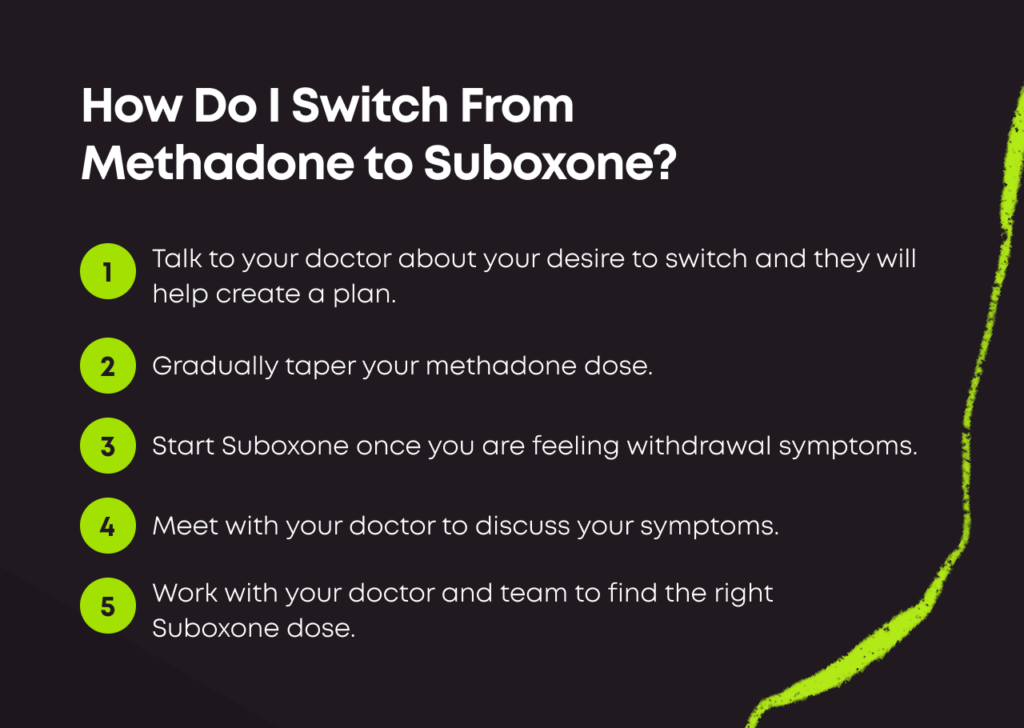
How Do I Switch From Methadone to Suboxone?
Transitioning from methadone to Suboxone requires careful medical supervision and detailed instructions. The following steps are involved:
1. Talk to Your Doctor
Moving from one MAT to another requires careful medical planning. Your buprenorphine doctor must assess several factors, including your current methadone dose, lifestyle and overall health. After an initial evaluation, your doctor will create a plan to help you move from one medication to another.
2. Taper Your Methadone Dose
The more methadone you take right now, the higher your risk of potential withdrawal. You and your doctor may decide to lower your methadone dose slowly before deciding to switch to Suboxone, or you may choose to change immediately from methadone to Suboxone without first tapering your methadone dose. This should be a decision you and your doctor make together.
3. Start Suboxone
Usually, it is recommended that patients stop methadone at least 36 hours before starting Suboxone. If Suboxone is taken too soon after methadone, it can cause precipitated withdrawal syndrome, which can make patients feel sick.
The best time to take your first dose of Suboxone is when you already feel like you are partially withdrawing from opioids. You may have symptoms like anxiety, fever or chills, sweating, shakiness, nausea, vomiting or diarrhea.
Plan to visit your doctor approximately one to two days after stopping methadone. They can monitor your symptoms and decide the best time for you to take your first dose of Suboxone.
4. Find the Right Dose of Suboxone
While methadone and Suboxone both treat OUD, the therapies work slightly differently. Finding the dose that’s right for you and your body can take time.
Be open and honest with your team about how you feel to make the experience as quick and efficient as possible. Your doctor may start you on a dose of Suboxone, monitor your symptoms and then increase or decrease your dose accordingly.
What Can I Expect When Transitioning From Methadone to Suboxone?
Moving from one medication to another could be right for you and your OUD. But the process can be uncomfortable, especially for people taking large doses of methadone.
Precipitated withdrawal involves the sudden appearance of significant symptoms like vomiting, diarrhea and bone pain due to starting Suboxone too soon after stopping methadone. There are ways to stop and prevent these uncomfortable symptoms at home, however, that can make it easier to switch medications.
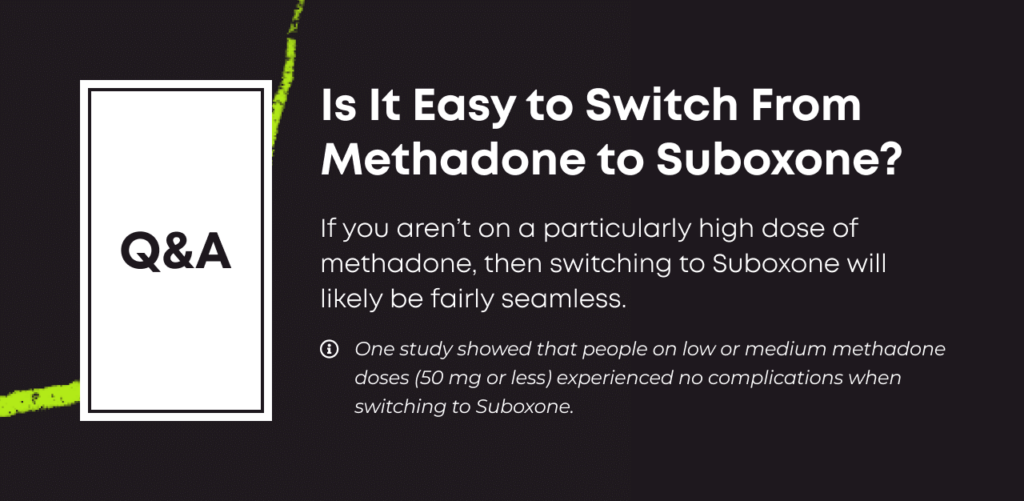
Conversely, if you aren’t on a particularly high dose of methadone, then switching to Suboxone will likely be fairly seamless. One study showed that people on low or medium methadone doses (50 mg or less) experienced no complications when switching to Suboxone.[6]
With proper supervision and support, you can avoid precipitated withdrawal. But you should expect to feel at least somewhat uncomfortable as you move from one therapy to another. Take time away from work, don’t plan anything stressful, and focus on completing the process as quickly and comfortably as possible.
If you aren’t on a particularly high dose of methadone, then switching to Suboxone will likely be fairly seamless. One study showed that people on low or medium methadone doses (50 mg or less) experienced no complications when switching to Suboxone.[6]
How Long After Taking Methadone Can I Take Suboxone?
When switching from methadone to Suboxone, you should ideally wait at least 24 hours after your last methadone dose before beginning Suboxone treatment. Your Suboxone doctor will recommend a starting dose and timeline according to your specific situation.
When switching from methadone to Suboxone, you should ideally wait at least 24 hours after your last methadone dose before beginning Suboxone treatment.
In a typical situation, people spend about a week switching from one medication to another. Discomfort is common and expected, so it’s best to avoid work and other social obligations as your body adjusts.
Your timeline involves the following:[7]
- Taper — timelines vary: You might first need to reduce your dose to about 30 mg of methadone per day. If you take a large amount of methadone for OUD, your taper may take longer.
- Cessation — up to 96 hours: You’ll stop taking any OUD medication. You’ll be uncomfortable during this time, with high relapse risks. Ensure you are talking to your doctor frequently and using friends and family for support to prevent any urge to relapse to opioid misuse during this time. It’s best if you aren’t alone during this period.
- Restart — 24 to 48 hours: You’ll start taking Suboxone under the guidance of a treatment team.
For some people, such as those on a low methadone dose, the switch from methadone to Suboxone can be just a few days or a week, while others who need to taper slowly off of a high methadone dose may need a few weeks to make the switch.
Methadone to Suboxone Dosing: Roughly Equivalent Doses
You’ll want to work closely with your doctor to figure out what Suboxone dose you should transition to based on your methadone dose, side effects, medication tolerance and more. However, below is a rough estimate of daily doses for each OUD medication. [10]
| Methadone | Buprenorphine |
| 10 mg | 2 mg |
| 20 mg | 4 mg |
| 30 mg | 6 mg |
| 40 mg | 8 mg |
| 60 mg | 12 mg |
| 80 mg | 16 mg |
How Hard Is It to Switch From Methadone to Suboxone?
Changing any kind of medication takes planning, patience and time.[8] Your body needs to adjust to the new medication. Side effects are common, and while they are never life-threatening, they may be extremely uncomfortable.
If you have the right level of support — both from your medical team and people in your life who care about you — switching from methadone to Suboxone is achievable. If you don’t have the right kind of support, or you don’t take the process seriously, you could struggle to switch.
Make this decision carefully, and ensure you’re fully prepared to see the process through. Have patience, and communicate openly with your care team during the transition period.
It can be challenging to switch from methadone to Suboxone, but the end result is very worth it for most patients. Most people experience some discomfort as they transition to Suboxone, and their risk for relapse is highest during the time period between their last methadone dose and their first Suboxone dose, but once they get through this, they enjoy the added convenience and ease of Suboxone as their form of MAT.
Online Suboxone Treatment With Bicycle Health
At Bicycle Health, we offer Suboxone treatment to people struggling with OUD. Our telemedicine model means patients don’t need to go to clinics or schedule in-person doctor appointments. You can do the work in the privacy of your home with access to staff around the clock when you need them.
We can help you make the switch to Suboxone from methadone, and we can supervise your recovery with MAT. Contact us to find out if our treatment protocols are right for you. We’re ready to help today.

Reviewed By Peter Manza, PhD
Peter Manza, PhD received his BA in Psychology and Biology from the University of Rochester and his PhD in Integrative Neuroscience at Stony Brook University. He is currently working as a research scientist in Washington, DC. His research focuses on the role ... Read More
- Trends in the Use of Methadone, Buprenorphine, and Extended-Release Naltrexone at Substance Abuse Treatment Facilities: 2003 to 2015. Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/sites/default/files/report_3192/ShortReport-3192.html. August 2017. November 2023.
- Drug Addiction Stigma in the Context of Methadone Maintenance Therapy: An Investigation into Understudied Sources of Stigma. International Journal of Mental Health and Addiction. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3743126/. February 2013. November 2023.
- Death Rate Maps and Graphs. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/deaths/index.html. June 2022. November 2023.
- Strategies for Transfer from Methadone to Buprenorphine for Treatment of Opioid Use Disorders and Associated Outcomes: A Systematic Review. Journal of Addiction Medicine. https://journals.lww.com/journaladdictionmedicine/Fulltext/2022/04000/Strategies_for_Transfer_From_Methadone_to.9.aspx. April 2022. November 2023.
- Transfer from Methadone to Buprenorphine. Providers Clinical Support System. https://pcssnow.org/wp-content/uploads/2014/03/PCSS-MATGuidanceTransferMethadonetoBup.Casadonte.pdf. May 2022. Accessed June 2023.
- Transferring Patients from Methadone to Buprenorphine: The Feasibility and Evaluation of Practice Guidelines. Journal of Addiction Medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5976217/. May 2018. Accessed November 2023.
- An Efficient and Smooth Methadone-to-Buprenorphine Transition Protocol Utilizing a Transdermal Fentanyl Bridge and a Pharmacokinetic Inducer: The Stanciu Method. Cureus. https://www.cureus.com/articles/32975-an-efficient-and-smooth-methadone-to-buprenorphine-transition-protocol-utilizing-a-transdermal-fentanyl-bridge-and-a-pharmacokinetic-inducer-the-stanciu-method. May 2020. Accessed November 2023.
- Effects of Medication Assisted Treatment (MAT) for Opioid Use Disorder on Functional Outcomes: A Systematic Review. Journal of Substance Abuse Treatment. https://www.journalofsubstanceabusetreatment.com/article/S0740-5472(17)30482-8/fulltext. March 2018. Accessed November 2023.
- Whelan PJ, Remski K. Buprenorphine vs methadone treatment: A review of evidence in both developed and developing worlds. J Neurosci Rural Pract. 2012;3(1):45-50. doi:10.4103/0976-3147.91934. Accessed November 2023.
- Vermont Buprenorphine Practice Guidelines. Vermont Department of Health. http://contentmanager.med.uvm.edu/docs/default-source/vchip-documents/vchip_2buprenorphine_guidelines.pdf?sfvrsn=2. Accessed November 2023.
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Related Content
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.
