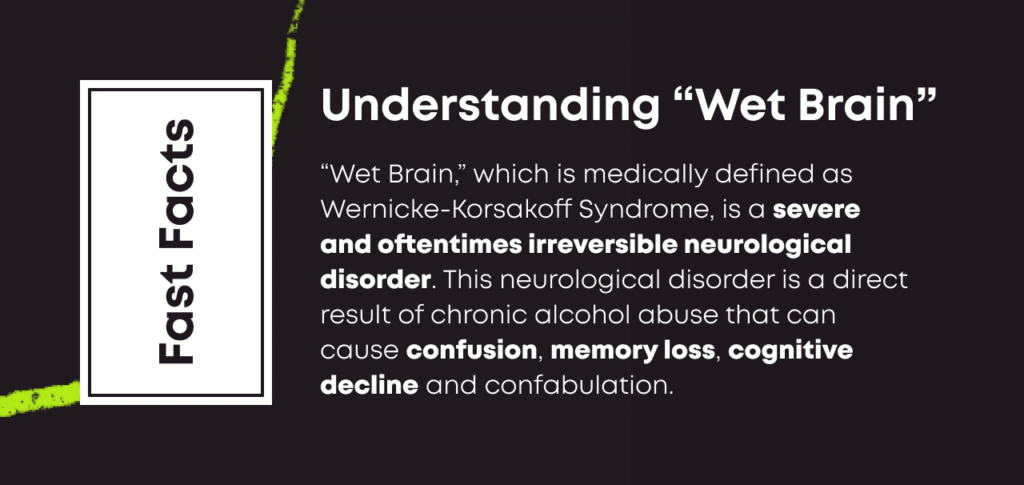
Wernicke-Korsakoff syndrome (WKS), colloquially referred to as “wet brain”, is a very serious condition that some people develop after chronic alcohol use disorder (AUD). Its causes are unknown and likely multifactorial, but it is likely in part due to a vitamin B1, or thiamine, deficiency.
This syndrome can cause significant, potentially permanent brain damage and lead to cognitive decline.
What Is “Wet Brain”?
Wet brain, which is known by medical experts as Wernicke-Korsakoff syndrome, is a condition that some people with long-term alcohol use disorder develop that can cause confusion, memory loss, confabulation and eventual cognitive decline.[1]
It is unknown exactly what causes WK syndrome, and it is likely multifactorial, but one likely contributing factor is vitamin B1 (thiamine) deficiency.
How Does Alcohol Cause “Wet Brain”?
Heavy drinking can result in inflammation of the stomach lining and digestive tract, affecting the body’s ability to absorb nutrients.[2] Additionally, patients with severe AUD may be drinking to such and extent that they are frequently vomiting or forgetting to eat regular meals, also contributing to nutrient deficiencies. Alcohol can also impact the ability of cells to utilize what thiamine is available.
Stages of Wernicke-Korsakoff Syndrome
Wernicke-Korsakoff syndrome can be further split into two distinct stages: Wernicke encephalopathy and Korsakoff syndrome.
Generally, a person will first develop symptoms of Wernicke encephalopathy, which is considered the first and potentially reversible stage of thiamine deficiency. It is often treatable with high doses of thiamine supplementation and, ideally, abstinence from alcohol.
In later stages of the cognitive decline, they will experience the symptoms of Korsakoff syndrome, which are by definition considered to be permanent, irreversible changes that respond poorly even to thiamine supplementation.
The symptoms of Wernicke encephalopathy include the following:
- Confusion, which can progress into coma and potentially result in death
- Loss of coordination, including potentially developing leg tremors
- Vision changes, including abnormal eye movements, double vision, and eyelid drooping
- Alcohol withdrawal
The symptoms of Korsakoff syndrome include the following:
- An inability to form new memories
- Progressive, severe memory loss
- Confabulation (making up stories that a person believes to be true)
- Auditory and visual hallucinations
All stages of Wernicke-Korsakoff syndrome should be taken seriously and warrant immediate medical attention. The sooner symptoms are addressed, the better a person’s prognosis.
Left untreated, a person with this condition who continues to drink may eventually be unable to function independently and may become severely cognitively impaired. Patients with this condition have a high mortality, both from brain disease as well as the often co-morbid failure of other body systems including the liver.
Treatment for Wernicke-Korsakoff Syndrome
Wernicke-Korsakoff syndrome is treated through the replacement of thiamine and proper levels of nutrition and hydration.[3] In addition, cessation of alcohol is the only real treatment long term.
It is important not to attempt treatment yourself and to seek help from medical professionals. A person with Wernicke encephalopathy is in a notably delicate condition and will need thiamine replacement treatments, ideally through an IV, usually requiring admission to the hospital.
Wernicke-Korsakoff Syndrome FAQs
How long can a person live with “wet brain”?
Life expectancy Wet brain, or Wernicke-Korsakoff syndrome, is highly variable. One study found over 50% of patients diagnosed with the condition are expected to die within 8 years.[4] Depending on the extent to which the patient has other comorbidities from alcohol – advanced liver disease, for example – the prognosis could be as short as months. Getting a diagnosis and treatment for thiamine deficiency as early as possible is the best way to increase the chance of survival.
How do you develop wet brain?
Wet brain is likely multifactorial but is in part triggered by nutritional deficiencies (thiamine) that are caused by long-term alcohol use. To minimize brain damage and prevent death, immediate medical treatment is needed.
Can you fully recover from wet brain?
Complete recovery from “wet brain” is unlikely. Most people will experience long-lasting changes to their memory and cognition even with treatment and abstaining from alcohol. However, partial recovery is possible. Many people see significant improvement in their symptoms if they take the appropriate measures recommended by doctors and abstain from alcohol.
Can you die from “wet brain”?
Yes, without treatment, cognitive decline can be severe enough that it’s possible to die from Wernicke-Korsakoff syndrome. You must stop drinking, get appropriate medical treatment, and avoid alcohol in the future.
Is “wet brain” like dementia?
In some ways, yes. Dementia is not a specific disease but a group of conditions involving cognitive decline over time. Wernicke-Korsakoff syndrome can cause many of the symptoms associated with dementia, including difficulty with thinking, memory, and reasoning. In terms of symptoms, it is reasonable to think of it as similar to dementia.
If you or someone you love has a history of heavy drinking and is experiencing behavioral changes concerning for memory loss or symptoms of dementia, it may be the time to intervene. Reach out to your medical team for help.

Medically Reviewed By Elena Hill, MD, MPH
Elena Hill, MD; MPH received her MD and Masters of Public Health degrees at Tufts Medical School and completed her family medicine residency at Boston Medical Center. She is currently an attending physician at Bronxcare Health Systems in the Bronx, NY where ... Read More
- Wernicke-Korsakoff syndrome. MedlinePlus. https://medlineplus.gov/ency/article/000771.htm. February 2020. Accessed August 2022.
- The Role of Thiamine Deficiency in Alcoholic Brain Disease. Alcohol Research & Health. https://pubs.niaaa.nih.gov/publications/arh27-2/134-142.htm. 2003. Accessed August 2022.
- Wernicke-Korsakoff Syndrome. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/wernicke-korsakoff-syndrome. July 2022. Accessed August 2022.
- Long-Term Mortality of Patients with an Alcohol-Related Wernicke-Korsakoff Syndrome. Alcohol and Alcoholism. https://pubmed.ncbi.nlm.nih.gov/28340112/. July 2017. Accessed August 2022.
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Related articles
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.