Suboxone is a prescription medication for opioid use disorder (OUD) that has helped countless people quit misusing opioids like heroin and prescription painkillers like Vicodin and Percocet. If you have OUD and use your medication as directed, addiction is extremely unlikely.
You may become physically dependent on your medication and feel unwell without it, but this is completely normal and expected. This means you won’t develop unhealthy behaviors typical of addiction (like lying about your medication or stealing to get more) to support your Suboxone use.
However, if you don’t have OUD and use Suboxone recreationally, you could develop an addiction. Treatment from a qualified team can help you get better.
How Does Suboxone Work?
Suboxone contains two ingredients to treat OUD: buprenorphine and naloxone. Buprenorphine is a partial opioid agonist that binds to opioid receptors in the brain and mitigates opioid cravings and withdrawal symptoms, decreases the risk of opioid overdose, and reduces the potential for misuse.[1]
Meanwhile, naloxone is an opioid antagonist, capable of rendering opioids inactive when people take too much or attempt to misuse the medication intravenously or intranasally.[2]
The medication is designed for at-home use, allowing people to take a daily dose without needing to head to a public clinic or hospital. Strips or tablets melt in the mouth, delivering powerful medication to ease symptoms of OUD.
Will Suboxone Get Me High?
If you take your Suboxone as prescribed, you won’t get high, although you may experience mild euphoria.[1] Suboxone intoxication in people with OUD is rare, experts say, and it’s typically caused by one of the following actions:[2]
- Combining Suboxone with other drugs
- Not following a doctor’s dosage directions
- Using Suboxone with stronger opioids
Because of naloxone, it’s almost impossible to overdose on Suboxone, improving safety considerably. But combining it with other drugs is never smart.
Is Suboxone Addictive?
People with OUD rarely develop an addiction to buprenorphine products like Suboxone. An OUD is characterized by compulsive drug use despite negative consequences. People tend to take more and more with little control over their doses. It’s nearly impossible for this to happen if someone with OUD takes Suboxone as prescribed by their doctor. Instead, they will experience relief from opioid cravings and withdrawal symptoms, which can help them to focus on things like therapy and long-term recovery.
Research indicates that about three-fourths of people using buprenorphine products don’t misuse them.[3]
Instead, they take them to keep their OUD symptoms under control.
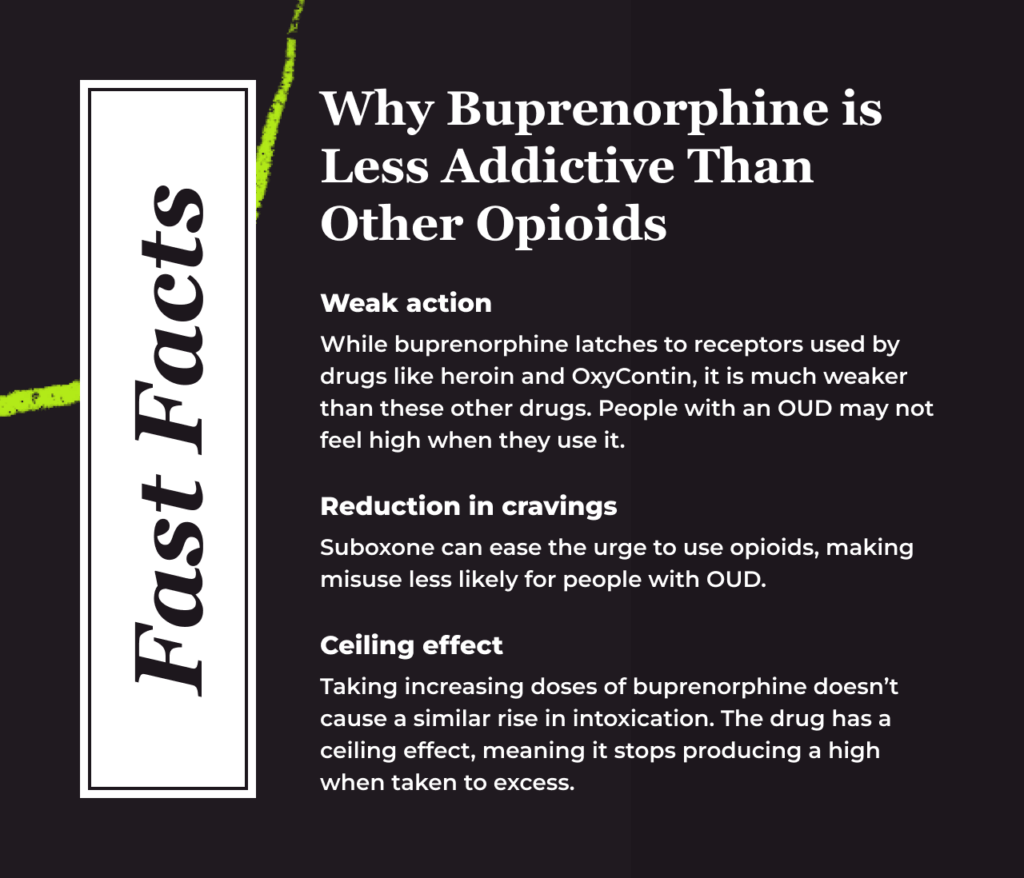
Buprenorphine is considered less addictive than other substances due to the following attributes:[4]
- Weak action: While buprenorphine latches to receptors used by drugs like heroin and OxyContin, it is much weaker than these other drugs. People with an OUD may not feel high when they use it.
- Reduction in cravings: Suboxone can ease the urge to use opioids, making misuse less likely for people with OUD.
- Ceiling effect: Taking increasing doses of buprenorphine doesn’t cause a proportionate rise in intoxication. The drug has a ceiling effect, meaning it stops producing a high when taken to excess.
The Difference Between Physical Dependence and Addiction
Long-term use of Suboxone can lead to physical dependence, which is a natural adaptation caused by ongoing use and doesn’t indicate an addiction to Suboxone. It simply means your body has adjusted to the presence of this medication.
When people feel in control of their OUD and want to stop taking Suboxone, doctors use tapering (slowly decreasing doses over a period of time) to help the body adjust. Quitting the medication cold turkey can lead to uncomfortable withdrawal symptoms, such as:[5]
- Nausea
- Vomiting
- Diarrhea
- Muscle aches
- Fever
- Excessive sweating
Physical dependence is not the same as addiction. Many people take Suboxone for years without misusing the medication in any way. But their bodies become accustomed to the presence of the drug, and they need help stopping their daily dose. Plenty of people remain on Suboxone indefinitely. As long as it is supporting your recovery, there’s no reason to stop taking it.
Signs of Suboxone Addiction
Although Suboxone addiction is rare, people with no history of OUD may occasionally misuse Suboxone for its potential pleasurable effects. A small number of people with OUD may also misuse their medication. Understanding what addiction looks like can allow you to offer help when needed.
People with Suboxone addiction may show the following signs:[5]
- Stealing money or objects for Suboxone
- Visiting multiple doctors to get Suboxone prescriptions
- Claiming their prescriptions were lost or stolen (so they can get more doses close together)
- Severe intoxication (drowsiness, slurred speech, slowed movements, memory or attention issues)
- Neglecting hobbies and responsibilities
As the OUD deepens, people may lose their jobs, relationships and financial health due to their Suboxone misuse.[5]
Again, though, Suboxone misuse and addiction are highly unlikely and this risk shouldn’t prevent you or a loved one from seeking Medication for Addiction Treatment (MAT). Suboxone is a life-saving medication that has shown many benefits, including increasing retention in treatment, reducing illicit opioid misuse and criminal activity, improving ability to gain and maintain employment, and improving survival.[6]
How Is Suboxone Addiction Treated?
Suboxone treatment typically involves both medications and therapy. Drugs like methadone can help soothe cravings, and since they’re given in supervised settings like clinics, misuse is much less likely. Therapy helps people uncover why they misused Suboxone and how their lives could be better if they quit.
With the right treatment program, people with Suboxone addiction can stop misusing the drug and feel better about their lives. The sooner they get started, the better.
Frequently Asked Questions About Suboxone Addiction Potential
How Long Does it Take to Get Addicted to Suboxone?
If you are taking your Suboxone as prescribed by your doctor, you won’t get addicted to Suboxone, even if you take it indefinitely. However, taking it every day can lead to physical dependence, which simply means your body has adjusted to Suboxone.
Can You Be Allergic to Naloxone?
Theoretically, you could be allergic or hypersensitive to naloxone and experience swelling of the lips or throat and hives, but no allergic reactions have been documented to date.[7],[8]
Can You Be Addicted to Suboxone?
Though rare, you can potentially become addicted to Suboxone if you misuse it for its euphoric and relaxing effects. However, Suboxone misuse is uncommon due to the ceiling effect of buprenorphine, buprenorphine’s weak opioid effects, and the naloxone causing precipitated withdrawal if someone attempts to inject the medication.

Reviewed By Peter Manza, PhD
Peter Manza, PhD received his BA in Psychology and Biology from the University of Rochester and his PhD in Integrative Neuroscience at Stony Brook University. He is currently working as a research scientist in Washington, DC. His research focuses on the role ... Read More
- Buprenorphine. Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/buprenorphine. January 2023. Accessed March 2023.
- Suboxone: Rationale, Science, Misconceptions. The Ochsner Journal. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5855417/. 2018. Accessed March 2023.
- Buprenorphine Misuse Decreased Among U.S. Adults with Opioid Use Disorder from 2015 to 2019. National Institute on Drug Abuse. https://nida.nih.gov/news-events/news-releases/2021/10/buprenorphine-misuse-decreased-among-us-adults-with-opioid-use-disorder-from-2015-2019. October 2021. Accessed March 2023.
- Buprenorphine: Potential for Abuse. U.S. Department of Justice. https://www.justice.gov/archive/ndic/pubs10/10123/10123p.pdf. September 2004. Accessed March 2023.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
- Medications for Substance Use Disorders (2023) Substance Abuse and Mental Health Services Administration. Available at: https://www.samhsa.gov/medications-substance-use-disorders (Accessed June 2023).
- Naloxone (2023) Substance Abuse and Mental Health Services Administration. Available at: https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/naloxone (Accessed: 01 June 2023).
- Does naloxone have any side effects? (2014) Working with BJA NTTAC. Available at: https://bjatta.bja.ojp.gov/naloxone/does-naloxone-have-any-side-effects (Accessed: 01 June 2023).
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Related Content
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.
