Between 2013 and 2019, deaths associated with synthetic opioids (like fentanyl) increased by 1,040%.[1] Dealers add fentanyl to drugs like heroin to maximize their profits and extend their supplies.[2] The next dose of drugs you buy could prove fatal, but quitting isn’t easy.
Chronic opioid misuse impairs your control of drug use, even when you understand the consequences. Even a slight dose reduction in any opioid you use regularly can trigger withdrawal symptoms and cravings. Most people return to opioid misuse when their discomfort grows severe.[3]
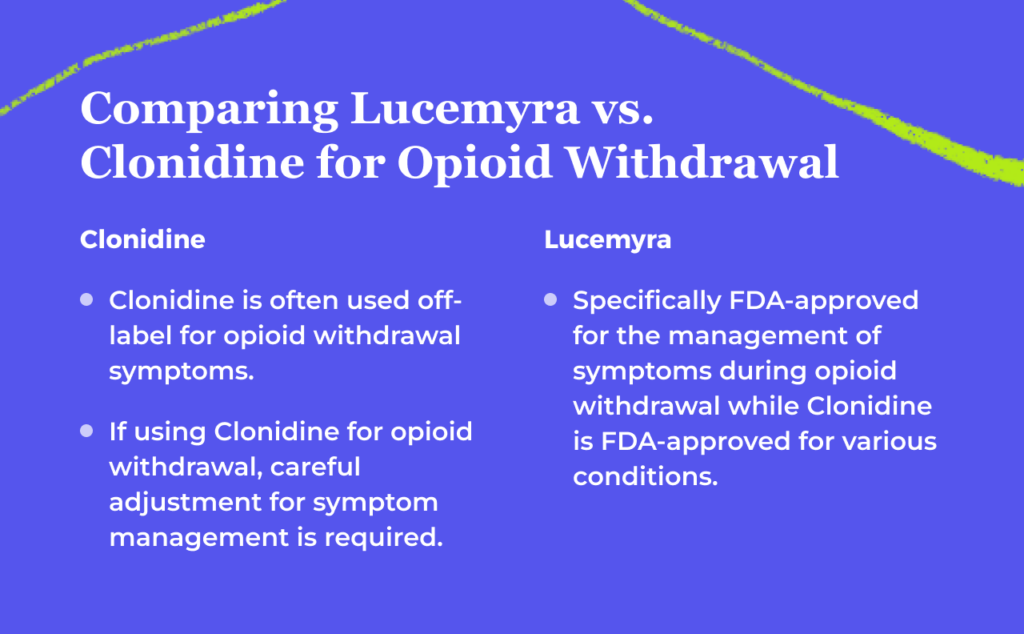
Treatment with medications can ease opioid withdrawal, so you can focus on rebuilding your life in recovery. Understanding Lucemyra vs. clonidine can help you determine which medication is right for your recovery.
Lucemyra vs. Clonidine: What’s the Difference?
Providing medications during opioid withdrawal reduces uncomfortable symptoms and increases the chances that you’ll stick with the process and avoid opioid misuse. Doctors have several options available, including Lucemyra and clonidine.
Both medications are alpha-2 adrenergic receptor agonists, not opioids. They suppress norepinephrine, which is commonly increased during withdrawal episodes. Your stress responses are reduced, leading to pain relief, sedation and lowered blood pressure.[3]
Clonidine is an older medication that’s U.S. Food and Drug Administration (FDA) approved for hypertension, ADHD, Tourette syndrome, and other health conditions. It’s not specifically designed for opioid withdrawal, but doctors sometimes lean on this 40-year-old medication for this purpose.[4]
Lucemyra is a brand-name formulation of lofexidine, which was FDA approved for opioid withdrawal in 2018.[5] No generic formulations are available, so it can be slightly more expensive than clonidine. The expense may be worthwhile, as studies suggest Lucemyra causes fewer uncomfortable side effects than clonidine.[3]
Understanding Lucemyra (Lofexidine) & How It Works
Lucemyra is the brand-name version of the generic drug lofexidine. It was FDA approved in 2018 to treat withdrawal symptoms caused by the abrupt discontinuation of opioids.[3]
The FDA approved other medications for opioid withdrawal before 2018. But these partial or full opioid agonists work differently than Lucemyra.
Instead of treating symptoms directly, drugs like methadone and buprenorphine latch to opioid receptors and “trick” the brain into believing it has access to the drugs it needs. Solutions like this can be very effective, but some people are uncomfortable with the idea of using a similar medication to treat opioid use disorders.
Lucemyra reduces norepinephrine within the bloodstream. The body releases this chemical during stressful situations, so it’s often elevated during withdrawal. Blocking this action can mean a slower heartbeat, less pain and increased relaxation.[3]
Since Lucemyra is not an opioid, it comes with no misuse risks. However, it can cause lowered blood pressure and fainting. People with underlying heart conditions may have worsening symptoms while using the medication.[5]
Quitting the drug abruptly can cause a strong increase in blood pressure. Tapering the amount is a safer option.[5] Always consult your doctor before you stop taking the medication or change your dose.
Understanding Clonidine & How It Works
Clonidine is a 40-year-old medication FDA approved for high blood pressure, ADHD, Tourette syndrome, and other conditions.[4] While clonidine is not specifically designed for opioid withdrawal, doctors have used it to reduce uncomfortable symptoms.
Clonidine lowers blood pressure and heart rate by reducing norepinephrine within the body. Clonidine can help people feel more relaxed, calm and comfortable.[4]
Unlike other opioid withdrawal medications, including methadone and buprenorphine, clonidine is not an opioid. It doesn’t latch to the same receptors or trigger any kind of sensations associated with opioids. As a result, its addiction risks are low.[4]
The medication can cause some uncomfortable side effects, including abdominal pain and nausea. Doses must also be tapered, instead of quitting abruptly, or rebound high blood pressure can develop.[4]
Lucemyra vs. Clonidine
| Lucemyra | Clonidine | |
| Drug type | Alpha-2 adrenergic receptor agonist | Alpha-2 adrenergic receptor agonist |
| Primary condition treated | Opioid withdrawal | Hypertension |
| Mechanism of action | Reduces norepinephrine | Reduces norepinephrine and increases blood flow |
| FDA approval date | 2018 | 1974 |
| Available formats | Tablet | Patch, tablet or injectable solution |
| Side effects | Low blood pressure, fainting and heartbeat irregularities | GI distress, headache, low blood pressure, sexual dysfunction, dizziness and sedation |
Treating Opioid Withdrawal: Which Medication Is Better?
Comparing Lucemyra vs. clonidine can help you understand which medication is best for you. Every person is different, so the one you pick could be different than the one another person uses. Here’s what you need to know:
Pros of Lucemyra
Advantages of Lucemyra include fewer potential side effects, including a smaller reduction in blood pressure when compared to clonidine. It’s specifically designed for opioid withdrawal and is FDA approved for that purpose.
Treatment typically lasts for about 14 days, and then, the dose tapers. People who don’t want to take drugs indefinitely may appreciate that fact.[3]
Cons of Lucemyra
Lucemyra’s main disadvantage involves cost. Since it’s a relatively new medication, no generic versions are available. It can be more expensive than clonidine. It’s also only available in tablet form, so people who don’t like pills may not appreciate this option.[3]
Pros of Clonidine
Advantages of clonidine include its lower cost and increased flexibility when compared to Lucemyra. You can use patches and injections, and generic forms could be less expensive than the brand-name versions.[4]
Cons of Clonidine
Disadvantages of clonidine include its effectiveness. Some studies suggest that clonidine isn’t as helpful in controlling symptoms, and some people struggle with powerful side effects like sedation.[6] While both drugs can lower blood pressure, clonidine is stronger and can cause more of these symptoms than Lucemyra does.[3]
Finding Treatment Options for Opioid Use Disorder
Quitting opioids abruptly is incredibly painful, and it’s rarely successful.[3] A Medication for Addiction Treatment (MAT) program is different.
In an MAT program, your team won’t rely on your willpower to help you stop using drugs. Instead, medications help to ease your withdrawal symptoms, so you can focus on rebuilding your life in therapy.
While Lucemyra and clonidine can reduce withdrawal symptoms, they don’t ease cravings. Your risk of relapse is very high with these drugs. MAT options like buprenorphine and methadone can ease withdrawal symptoms, and you can keep taking them indefinitely to reduce your relapse risks. Many people take them for years, decades, or even for the rest of their lives.
At Bicycle Health, we use Suboxone for MAT. This medication combines buprenorphine with naloxone (a misuse deterrent). You can use this medication at home, without going to a clinic every day.
Some people use Suboxone in concert with Lucemyra or clonidine. But others use Suboxone alone, without any other medications. Your Bicycle Health team can help you understand which choice is right for you. While the team doesn’t prescribe or administer Lucemyra or clonidine, your Suboxone program can be administered by Bicycle Health.

Reviewed By Peter Manza, PhD
Peter Manza, PhD received his BA in Psychology and Biology from the University of Rochester and his PhD in Integrative Neuroscience at Stony Brook University. He is currently working as a research scientist in Washington, DC. His research focuses on the role ... Read More
- Mattson C, Tanz L, Quinn K, Kariisa M, Patel P, Davis N. Trends and geographic patterns in drug and synthetic opioid overdose deaths—United States, 2013-2019. Morbidity and Mortality Weekly Report. 2021;70(6):202-207. https://www.cdc.gov/mmwr/volumes/70/wr/mm7006a4.htm?s_cid=mm7006a4_w
- 2020 national drug threat assessment. U.S. Drug Enforcement Administration. Published March 2021. Accessed December 1, 2023. https://www.dea.gov/sites/default/files/2021-02/DIR-008-21%202020%20National%20Drug%20Threat%20Assessment_WEB.pdf
- Urits I, Patel A, Zusman R, Virgen C, Mousa M, Berger A, et al. A comprehensive update of lofexidine for the management of opioid withdrawal symptoms. 2020;50(3):76-96. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7377538/
- Yasaei R, Saadabadi A. Clonidine. StatPearls. Published July 17, 2023. Accessed December 1, 2023. https://www.ncbi.nlm.nih.gov/books/NBK459124/
- Lucemyra prescribing information. U.S. Food and Drug Administration. Published 2018. Accessed December 1, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/209229s000lbl.pdf
- Gerra G, Zaimovic A, Giusti F, Gennaro C, Zambelli U, et al. Lofexidine versus clonidine in rapid opiate detoxification. Journal of Substance Abuse Treatment. 2021;21(1):11-7. https://pubmed.ncbi.nlm.nih.gov/11516922/
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Related Content
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.