Sublocade withdrawal isn’t usually intense, but symptoms can be managed with a tapered approach to stopping use.
Sublocade contains a long-lasting form of buprenorphine.[2] It’s designed to take action slowly and wear off gently.
Most people don’t notice severe withdrawal symptoms when they quit using it. If you do feel sick, symptoms might appear within a few weeks of your last dose.
To ensure you don’t experience Sublocade withdrawal, your doctor might suggest a buprenorphine taper. Taking smaller doses over long periods could help your body gradually adjust to the absence of buprenorphine.
What Is Sublocade?
Sublocade is an injectable form of buprenorphine that lasts for about a month. Doctors use shots to help people overcome opioid use disorder (OUD). Medication for Addiction Treatment (MAT) is an effective way to help people quit using drugs for good.[3]
In Sublocade studies, close to half of participants maintained sobriety for 18 months.[1] With one monthly shot, they were able to quit misusing opioids for good.
Unlike other forms of buprenorphine, Sublocade is administered in doctor’s appointments. You can’t take the drug home. For people concerned about a temptation to misuse the medication, Sublocade could be a good option.
How Long Does Sublocade Stay in Your System?
Sublocade stays active within your system for 43 to 60 days after each injection.[2] Most people get shots every month, ensuring they don’t experience higher relapse risks.
If you take Sublocade for four to six months, buprenorphine remnants will remain in your body (and detectable in drug tests) for up to a year.[1] You may not notice the drug working, but you can fail a drug test designed to detect buprenorphine. Make sure to tell any testing administrator about your past use of Sublocade or any other form of buprenorphine.
Since buprenorphine in Sublocade remains in your body for so long, few people experience withdrawal symptoms when they stop using the drug. But if you’ve only used Sublocade for a month or two, you could feel sick if you skip your doses.
What to Expect From Sublocade Withdrawal
Doctors are encouraged to monitor their MAT patients for signs of withdrawal if they quit Sublocade abruptly.[2]
Classic buprenorphine withdrawal follows this timeline:[4]
- Within 48 hours of the last dose: Withdrawal symptoms may start to appear.
- Within three days: Symptoms peak in intensity.
- Within 10 days: Symptoms fade.
Sublocade’s long-lasting action extends this timeline. You may not feel symptoms for weeks instead of days.
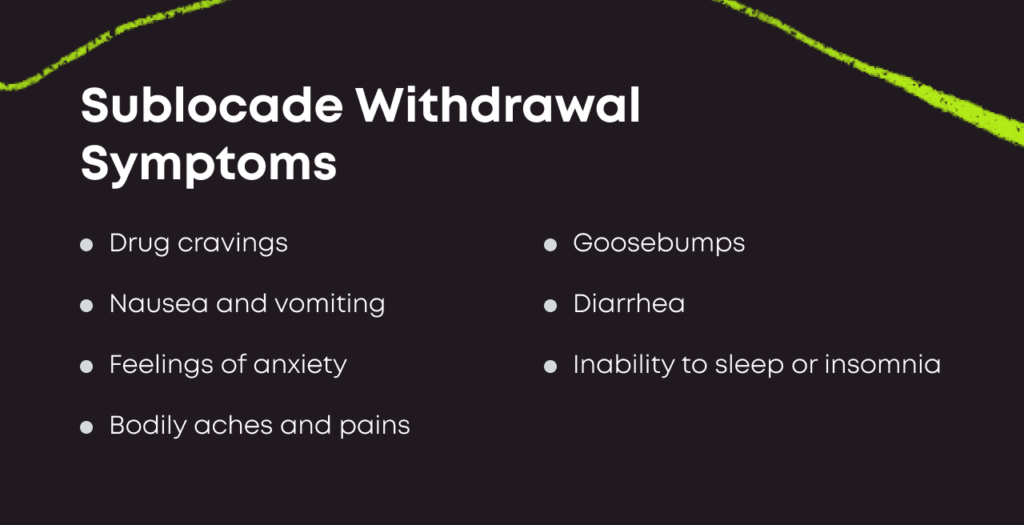
Potential withdrawal symptoms to expect include the following:[2]
- Nausea
- Vomiting
- Diarrhea
- Drug cravings
- Aches and pains
- Goosebumps
- Insomnia
- Anxiety
Your doctor will monitor you for several months to ensure you don’t experience severe symptoms.[2] Extreme discomfort increases your risk of relapse. Because of this, your doctor will guide you through the withdrawal process, aiming to minimize symptoms to guard against relapse.
How Is Sublocade Withdrawal Treated or Prevented?
Sublocade withdrawal can be serious, as it increases your risk of returning to drugs like heroin and OxyContin. If you experience symptoms, tell your doctor. And if you’re considering quitting your treatment plan, talk to your doctor first.
Preventing Sublocade withdrawal might involve these steps:[2]
- Switching medications: Your doctor may offer an oral buprenorphine medication when your last shot begins to wear off. This may be in the form of a tablet or film strip.
- Monitoring your progress. You adjust to the new drug and don’t experience discomfort or sickness over time.
- Tapering your dose: Your doctor creates a plan to help you take less of the medication without feeling sick. You may continue to taper your dose until you are no longer using the medication at all.
If you experience Sublocade withdrawal, your doctor might follow these same steps to help you feel better. In some cases, you might enter a detox program and access medications to treat your symptoms as your body adjusts. The severity of your symptoms will dictate your doctor’s approach.
Is Withdrawal the Same as Addiction?
Your body becomes physically dependent on buprenorphine after long-term exposure. But physical dependence is not the same as addiction.[5]
People who are physically dependent on a medication feel sick without it. With treatment, they can overcome this sickness and allow their bodies to return to a normal level of functioning.
People who are addicted to a substance are both physically and psychologically attached to a substance. They put the drug at the center of their lives, developing habits to support and sustain the addiction. This illness can be life-threatening.
If you’re physically dependent on Sublocade, you may feel sick when you quit. But know that this is not a sign of addiction. And it’s not a condition that will stay with you forever.
Finding Addiction Treatment for OUD
MAT programs can help you break your connection with drug misuse. Bicycle Health offers an innovative telemedicine program to bring the power of MAT into your home. Visit with our doctors via video chat, pick up your prescription at a local pharmacy and start on the path to a new life.
Bicycle Health uses Suboxone in our MAT program. Suboxone contains buprenorphine (for OUD recovery) and naloxone (for misuse prevention). When combined, these medications allow for safe at-home delivery.
Take your medications in the privacy of your home, and stay connected with your doctor via telemedicine. We work with most insurance providers, and we make enrollment quick and easy. Contact us to find out if this model is right for you.

Reviewed By Peter Manza, PhD
Peter Manza, PhD received his BA in Psychology and Biology from the University of Rochester and his PhD in Integrative Neuroscience at Stony Brook University. He is currently working as a research scientist in Washington, DC. His research focuses on the role ... Read More
- Boyett B, Nadipelli VR, Solem CT, Chilcoat H, Bickel WK, Ling W. Continued Posttrial Benefits of Buprenorphine Extended Release: RECOVER Study Findings. J Addict Med. 2023;17(2):182-189. doi:10.1097/ADM.0000000000001070
- Sublocade prescribing information. U.S. Food and Drug Administration. Published March 2021. Accessed August 16, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/209819s017s018lbl.pdf
- Maglione MA, Laura R, Christine C, et al. Effects of Medication-Assisted Treatment (MAT) for Opioid Use Disorder on Functional Outcomes: A Systematic Review. Rand Health Q. 2020;8(4):RR-2108-OSD. Published 2020 Jun 15
- Tripathi BM, Hemaraj P, Dhar NK. Buprenorphine withdrawal syndrome. Indian J Psychiatry. 1995;37(1):23-25.
- Szalavitz M, Rigg KK, Wakeman SE. Drug dependence is not addiction-and it matters. Ann Med. 2021;53(1):1989-1992. doi:10.1080/07853890.2021.1995623
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.