Generally, you should avoid the use of hydrocodone (Norco, Vicodin) and other opioids if you are taking Suboxone (buprenorphine/naloxone). However, there are instances, such as surgery, where your doctor may recommend managed opioid use to control acute pain.
Healthcare professionals are hesitant when it comes to prescribing opioids like hydrocodone to individuals receiving Suboxone therapy for opioid use disorder (OUD). This is due to the fact that both drugs are opioid agonists, which could cause dangerous side effects. Plus, Suboxone dulls the effects of other opioids like hydrocodone, making it less effective in relieving pain.
Nevertheless, there may be particular instances where a healthcare provider may choose to combine these drugs for pain management purposes. This will normally only occur under close observation and when certain conditions are met.
Can you take Norco and Suboxone together?
Quick Answer
You should never take Norco and Suboxone without being directed to by a doctor. Combining these opioids could lead to harmful and life-threatening consequences, such as respiratory depression and overdose. This is especially true if you are misusing Norco in any way. Suboxone blocks the effects of other opioids like hydrocodone so you may wind up taking a high dose to overcome the blocked effects, ultimately leading to coma, overdose, and even death.
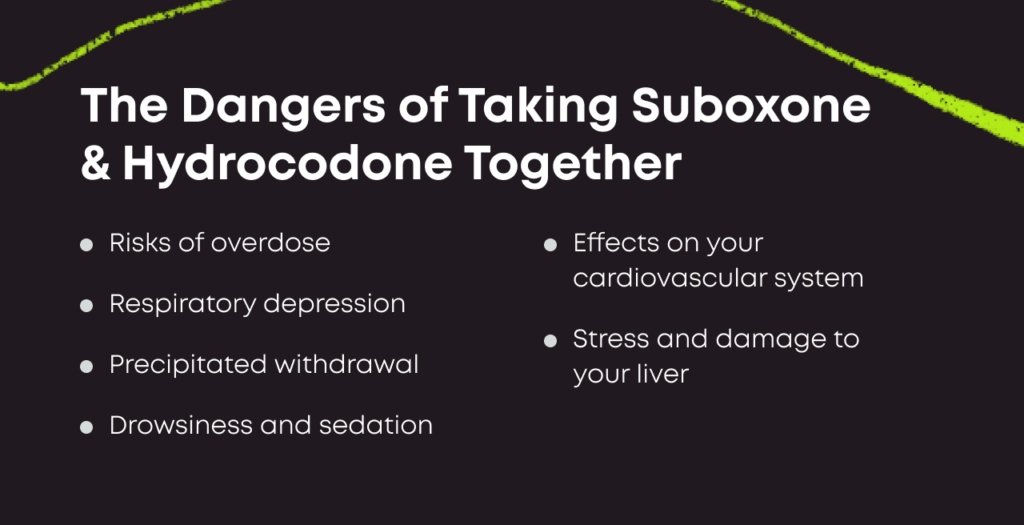
What Are the Dangers of Taking Hydrocodone & Suboxone Together?
For those who are receiving treatment for opioid use disorder through medications like Suboxone, there are risks associated with taking additional opioids like hydrocodone.[2] Typically referred to as a full opioid agonist, hydrocodone has been linked with addictive behaviors and misuse tendencies.
Risk of Opioid Overdose
If you are taking Suboxone and misuse hydrocodone to get high, you may experience reduced euphoria. When hydrocodone is taken medically alongside Suboxone, it can result in significantly weaker pain relief than when hydrocodone is taken alone.[3]
This is because buprenorphine has a stronger affinity to opioid receptors than other opioids, essentially blocking the effects of Vicodin and Norco. In an attempt to overcome these blocked effects, people may misuse high doses of hydrocodone, which could lead to an opioid overdose.
Signs and symptoms of an opioid overdose include: [2]
- Drowsiness
- Slowed heartbeat
- Slowed or stopped breathing
- Difficulty breathing
- Cold, clammy skin
- Blue-ish lips and fingernails
- Muscle weakness
- Unresponsiveness
Combining these two medications also increases the risk of respiratory depression due to their shared effects on brain receptors. This can lead to potentially fatal outcomes like coma or death in the worst cases.[4]
Individuals receiving OUD treatment through Suboxone are usually encouraged to avoid potent opioids like hydrocodone due to their potential for causing relapse. Both patients and healthcare providers alike must work together to monitor use closely and prevent misuse.
When Would Doctors Recommend Taking Both?
While it is not usual practice for someone to take both hydrocodone and Suboxone at the same time, because they are both opioids with the potential for dangerous interactions, there are instances when an individual may need them under close supervision from a healthcare professional.[5]
Chronic Pain Management
For instance, if hydrocodone was initially prescribed for managing chronic pain but resulted in opioid dependence over time, switching to Suboxone could help to manage OUD while some level of hydrocodone use is still used for providing pain relief. This would only be done via carefully monitored medication use and dosage adjustments.
Short-Term Severe Pain
Opioids often represent the only option for the effective treatment of especially severe pain.[6] Even if a person has OUD, it is sometimes necessary for a doctor who is aware of this to still prescribe opioids (although likely with much more oversight than is standard) if no non-opioid solution can keep that individual from experiencing debilitating levels of pain. In such cases, a person might be put on a drug like hydrocodone even if currently taking Suboxone as part of a Medication for Addiction Treatment (MAT) program.
Surgical Procedures
It used to be that patients on MAT were advised to stop the use of Suboxone or buprenorphine prior to surgery. That is no longer the recommendation. Now, it’s recommended that patients remain on their MAT prior to surgery.[7]
In some cases, the dose of Suboxone or buprenorphine may be raised to provide pain control or the dose may be divided up throughout the day differently. Doctors may prescribe a short-acting full opioid agonist, like hydrocodone, to control acute pain, but again, this is closely monitored.[8]
It must be noted that taking these medications without proper medical oversight can have severe consequences like overdose or other detrimental effects on health.
Alternate Options to Hydrocodone & Other Opioids for Acute Pain
Some alternatives to hydrocodone for acute pain include over-the-counter (OTC) pain medications, such as:[9]
- Naproxen (Aleve)
- Aspirin (Bayer)
- Acetaminophen (Tylenol)
- Ibuprofen (Advil, Motrin)
You can also use OTC topical medications for pain relief, such as:
- Capsaicin gels or creams
- Menthol gels or creams
- Salicylate creams
- Lidocaine creams or patches
These OTC drugs aren’t opioids and don’t have potential for misuse or addiction. While they aren’t as potent as opioids, they can still help with pain and are especially useful in cases where a patient may be experiencing mild to moderate pain rather than severe pain.
Still, OTC medications for alleviating pain come with some potential side effects, which might make them unsuitable for use by some. Patients affected by liver or kidney ailments can experience complications when using acetaminophen, while those battling stomach ulcers might display an intolerance toward ibuprofen and naproxen.
Maintaining a balance between following recommended doses without overdoing them is important even with OTC medication that doesn’t require a prescription. Using them beyond their recommended limits could prove detrimental to your health.
Seek Medical Advice Before Taking Hydrocodone With Suboxone
As a general rule, do not take hydrocodone or any opioid while you are taking Suboxone. Since you are taking Suboxone for OUD, any use of hydrocodone that is not directed by a doctor qualifies as misuse and threatens your recovery. This is putting aside the fact that hydrocodone is only legally available through prescription, so the only legitimate way to start using it is by consulting a professional regardless.
Your goal when working with a medical professional is to find a workable solution to your pain. Talk with the doctor about why you think you might need an opioid painkiller and listen if they present alternate solutions that may allow you to avoid opioids altogether. Your doctor may also recommend non-medication approaches, such as:[10]
- Physical therapy
- Yoga
- Massage
- Electrostimulation
While non-opioid solutions may not always provide the needed pain relief, they can still be a valuable tool for combating pain. They should at least be tried if opioid use is likely to be especially dangerous or ineffective because you’re on Suboxone.
How Suboxone Works
Suboxone provides a viable path to recovery for those grappling with opioid use disorder (OUD).[1] Made of buprenorphine and naloxone, Suboxone diminishes opioid cravings and withdrawal symptoms.
Buprenorphine works by binding to opioid receptors in the brain without causing powerful euphoria or significant respiratory depression, unlike other opioids such as heroin or oxycodone. This action reduces dependence on opioids while stabilizing brain chemistry.
Sublingual tablets or films are the usual forms for administering Suboxone. These are dissolved under the tongue for faster absorption into the bloodstream. Often paired with therapy and counseling, Suboxone and similar drugs have helped many people successfully combat opioid use disorder across America.

Reviewed By Peter Manza, PhD
Peter Manza, PhD received his BA in Psychology and Biology from the University of Rochester and his PhD in Integrative Neuroscience at Stony Brook University. He is currently working as a research scientist in Washington, DC. His research focuses on the role ... Read More
- Buprenorphine. Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/buprenorphine. March 2023. Accessed April 2023.
- Hydrocodone. U.S. National Library of Medicine. https://medlineplus.gov/druginfo/meds/a614045.html. January 2021. Accessed April 2023.
- Buprenorphine/Naloxone Therapy in Pain Management. Anesthesiology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3999180/. May 2014. Accessed April 2023.
- Basic Opioid Pharmacology: An Update. British Journal of Pain. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4590096/. February 2012. Accessed April 2023.
- Perioperative Management of a Patient Taking Suboxone® at the Time of Ambulatory Surgery. Case Reports in Anesthesiology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7085354/. March 2020. Accessed April 2023.
- Acute Pain Management for Patients Receiving Maintenance Methadone or Buprenorphine Therapy. Annals of Internal Medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1892816/. January 2006. Accessed April 2023.
- Treating Perioperative and Acute Pain in Patients on Buprenorphine: Narrative Literature Review and Practice Recommendations. Journal of General Internal Medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7728902/. August 2020. Accessed April 2023.
- MCSTAP Learning Case: Acute Pain Management for Patient on Suboxone. MCSTAP. https://www.mcstap.com/docs/Acute%20Pain%20Management%20for%20Patient%20on%20Suboxone.pdf. Accessed April 2023.
- Successful Pain Management for the Recovering Addicted Patient. The Primary Care Companion to the Journal of Clinical Psychiatry. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC315480/. 2002. Accessed April 2023.
- Using TENS for Pain Control: The State of the Evidence. Pain Management. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4186747/. May 2014. Accessed April 2023.
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Related Content
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.