- What Is Precipitated Withdrawal?
- How Long Does Precipitated Withdrawal Last?
- What Medications Can Trigger Precipitated Withdrawal?
- Precipitated Withdrawal Symptoms & Their Duration
- Why Does Precipitated Withdrawal Happen?
- How Is Precipitated Withdrawal Best Treated/Prevented?
- How Common Is Precipitated Withdrawal?
- Precipitated Withdrawal FAQs
Precipitated withdrawal involves opioid withdrawal symptoms that are “precipitated” or brought on by taking an opioid antagonist (naltrexone, naloxone, or Vivitrol) or a partial opioid agonist (buprenorphine) too soon after taking a full opioid agonist (heroin, oxycodone, morphine, etc.).
Precipitated withdrawal can last for hours or even days, depending on the severity of the individual’s opioid use disorder, the medication that induced withdrawal, their withdrawal history, and whether they receive treatment for the precipitated withdrawal (OUD). [1]
In order to prevent precipitated withdrawal when taking a new medication like Suboxone or naltrexone, talk with your doctor and let them know the last time you used any opioids prior to starting these medications.
How Long Do Precipitated Withdrawal Symptoms Last?
Quick Answer
Precipitated withdrawal symptoms can last for anywhere from a few hours to a couple of days, depending on the severity of opioid dependence, the medication that induced withdrawal, their withdrawal history and whether they receive treatment for the withdrawal symptoms.
What Is Precipitated Withdrawal?
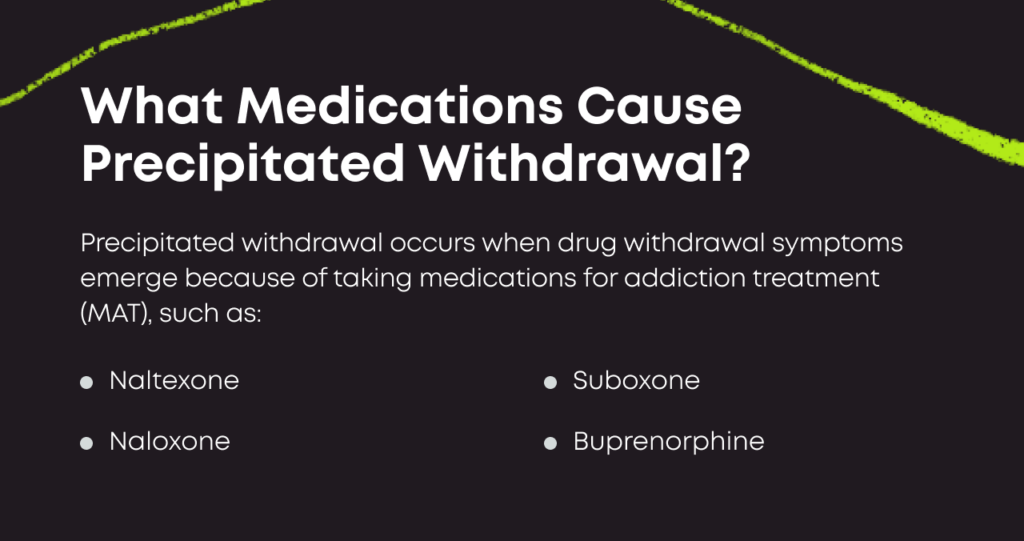
Precipitated withdrawal occurs when drug withdrawal symptoms emerge because of taking medications for addiction treatment (MAT), such as:
- Naltrexone
- Naloxone
- Suboxone
- Sublocade
- Vivitrol
- Other buprenorphine medications
The symptoms themselves are the same as the symptoms of natural withdrawal from opioids—when a person abruptly stops taking the drug—but these might come on more quickly.
Timeline: How Long Does Precipitated Withdrawal Last?
Some people experience precipitated withdrawal for just a few hours. Others may have symptoms for days.
The specific timeline will vary according to many factors, such as:
- The severity of dependence
- Previous withdrawal experiences
- The specific medication that induced withdrawal
- The dose of the medication
- Treatment and support
What Medications Can Trigger Precipitated Withdrawal?
Precipitated withdrawal is associated with opioid use disorder and medications for addiction treatment. Three common drugs might trigger precipitated withdrawal.
Naloxone
Naloxone (Narcan) is an opioid antagonist that binds to opioid receptors in the brain and blocks the effects of opioids of misuse like fentanyl and heroin. It rapidly reverses the life-threatening effects of an opioid overdose so the person has time to receive emergency medical care. The half-life of this medication is far less than that of many full opioid agonists, so the effect is temporary. [2]
However, they will experience precipitated withdrawal symptoms temporarily while the medication is working. And though these symptoms can be uncomfortable, they aren’t life-threatening the way that an opioid overdose is.
Naltrexone (Vivitrol)
Naltrexone is also an opioid antagonist but lasts far longer than naloxone and has very different prescription uses.
Naltrexone is not prescribed to stop overdoses. Instead, it is taken regularly to prevent intoxication or euphoria in the event of a relapse.[3]
Naltrexone binds to the opioid receptors in the brain for either hours or days, depending on the dose and formula. If the individual relapses and takes opioids, they will not experience the pleasurable effects or sedation while naltrexone is active in the body.
To start naltrexone treatment, a person must completely stop taking any opioid, including buprenorphine or methadone. If opioids are still in the bloodstream, naltrexone will stop all their effects on the brain, which can induce precipitated withdrawal.[4]
Buprenorphine, Suboxone, and Sublocade
Buprenorphine is a partial opioid agonist medication typically prescribed to treat opioid use disorder. And Suboxone is a combination medication comprised of buprenorphine and naloxone, and Sublocade is the monthly injectable version.
Buprenorphine, although it is a relatively weak opioid, has a high affinity for a specific opioid receptor; which means that it displaces opioids of misuse like fentanyl or heroin from receptors. This leads to precipitated withdrawal.[5]
Doctors who prescribe buprenorphine treatment for opioid use disorder stress the importance of ensuring an individual has stopped taking opioid drugs like heroin or prescription painkillers long enough before beginning treatment to avoid precipitated withdrawal.
Precipitated Withdrawal Symptoms
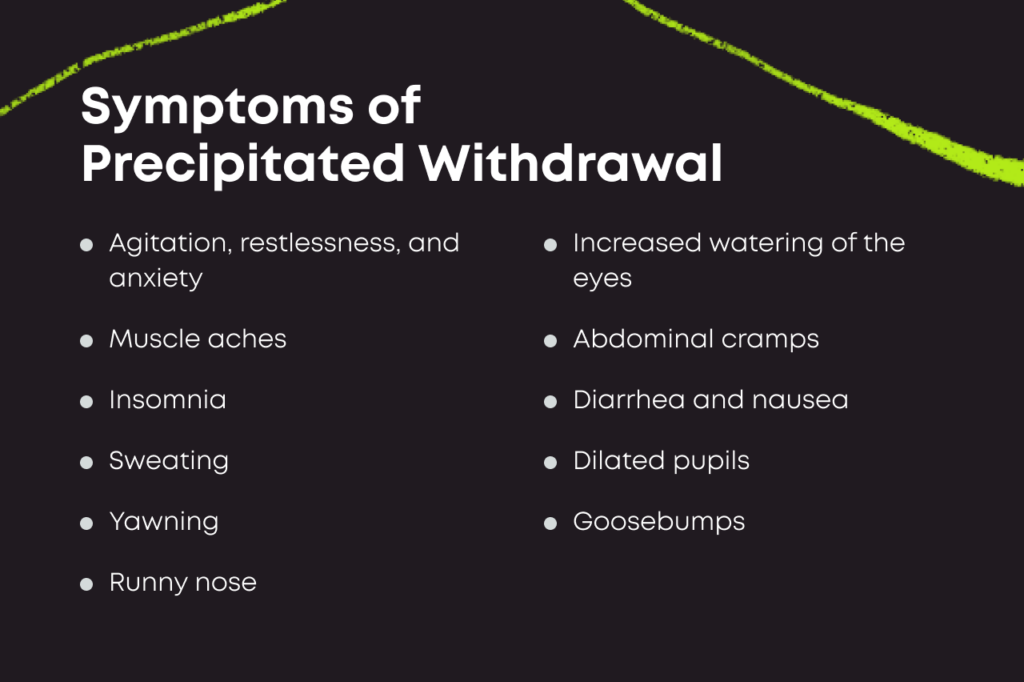
Symptoms associated with precipitated withdrawal are like acute opioid withdrawal, but they typically occur faster and feel more intense. Precipitated withdrawal symptoms include the following: [6]
- Agitation, restlessness, and anxiety
- Muscle aches
- Increased watering of the eyes
- Insomnia
- Sweating
- Yawning
- Runny nose
- Abdominal cramps
- Diarrhea and nausea
- Dilated pupils
- Goosebumps[6]
With treatment, including continuing Suboxone treatment, precipitated withdrawal can be managed safely. However, its onset can be very disruptive.
Why Does Precipitated Withdrawal Happen?
There are different reasons depending on the medication. When it comes to an opioid agonist like buprenorphine, it binds to opioid receptors in the brain more strongly than full opioid agonists, such as heroin, fentanyl, Percocet, Vicodin, and beyond.
This may sound a little counterintuitive, but buprenorphine actually has a stronger affinity for these receptors, which means it displaces the other opioids, leading to precipitated withdrawal.
As for opioid antagonists like naltrexone and naloxone, they bind to opioid receptors in the brain, blocking the effects of opioids of misuse. This blocking effect sends people into immediate withdrawal.
How Is Precipitated Withdrawal Best Treated/Prevented?
The best way to stop precipitated withdrawal is simply prevention: Make sure not to take a partial opioid agonist like buprenorphine or an antagonist like naloxone or naltrexone too soon after taking a full opioid agonist.
If you do experience withdrawal, either natural or precipitated, there are some adjunctive medications that can help to ease symptoms, including: [7], [8]
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or acetaminophen
- Antiemetics to reduce nausea and vomiting
- Clonidine to manage blood pressure
- Lofexidine to manage sickness from opioid withdrawal
Additionally, you may be able to call your doctor to get prescribed an opioid withdrawal medication, such as buprenorphine. Although buprenorphine can cause precipitated withdrawal, it can also mitigate the symptoms.
How Common Is Precipitated Withdrawal?
Fortunately, with buprenorphine treatment, the likelihood of precipitated withdrawal is low, particularly if you follow your doctor’s guidance.[9]
When precipitated withdrawal from buprenorphine does occur, it is often mild and brief.
If you follow your doctor’s directions closely, the process of beginning Suboxone therapy is quite manageable, and precipitated withdrawal is of little concern. Suboxone is a very safe and effective treatment that has helped millions of people reclaim their lives from opioid use disorder.
Precipitated Withdrawal FAQs
How long does precipitated withdrawal last?
Everyone’s a little different, but most people move through precipitated withdrawal in just a few hours, although it can last up to 48 hours.
Why does buprenorphine cause precipitated withdrawal?
Buprenorphine is a partial opioid agonist, capable of binding to receptors used by heroin and prescription painkillers. Take a dose, and it can displace stronger drugs from their attachments and trigger withdrawal. This is called “precipitated” withdrawal when the symptoms are induced by taking a drug.
How long do I have to wait to take Suboxone?
Your wait times can vary, depending on what opioids you took, how long you’ve used drugs, and how quickly your body processes drugs. Your treatment team can tell you how long you should wait to take Suboxone. The recommended period between stopping full opioids and starting a partial opioid agonist or antagonist is usually somewhere between 12 to 48 hours.

Reviewed By Peter Manza, PhD
Peter Manza, PhD received his BA in Psychology and Biology from the University of Rochester and his PhD in Integrative Neuroscience at Stony Brook University. He is currently working as a research scientist in Washington, DC. His research focuses on the role ... Read More
- A Case of Buprenorphine-Precipitated Withdrawal Managed With High-Dose Buprenorphine. Family Practice. https://pubmed.ncbi.nlm.nih.gov/34173647/. March 2022. Accessed September 2022.
- Naloxone Drug Facts. National Institute on Drug Abuse. https://nida.nih.gov/publications/drugfacts/naloxone. January 2022. Accessed September 2022.
- Naltrexone. National Library of Medicine. https://medlineplus.gov/druginfo/meds/a685041.html. October 2017. Accessed September 2022.
- Opioid Withdrawal Precipitated by Long-Acting Antagonists. The Journal of Emergency Medicine. https://www.jem-journal.com/article/S0736-4679(19)31117-5/fulltext. February 2020. Accessed September 2022.
- Fact Sheet: Buprenorphine. University of Massachusetts. https://www.umassmed.edu/globalassets/center-for-integrated-primary-care/amber/final-fact-sheet-on-buprenorphine-final.pdf. Accessed September 2022.
- Opiate and Opioid Withdrawal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/000949.htm. May 2020. Accessed September 2022.
- Frequently Asked Questions About ED-Initiated Buprenorphine. National Institute on Drug Abuse. https://nida.nih.gov/nidamed-medical-health-professionals/discipline-specific-resources/emergency-physicians-first-responders/initiating-buprenorphine-treatment-in-emergency-department/frequently-asked-questions-about-ed-initiated-buprenorphine. September 2019. Accessed September 2022.
- Lofexidine. U.S. National Library of Medicine. https://medlineplus.gov/druginfo/meds/a618036.html. August 2018. Accessed September 2022.
- Pharmacological Treatment for Drug Use Disorders. Treat.Net. https://www.unodc.org/documents/treatnet/Volume-C/Module-2/Volume_C_M2_W3.pdf. Accessed September 2022.
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.