When Spiderman 3 (No Way Home) broke box office records last Christmas, theater-lovers hoped it was a sign that Covid fears were over and that the movie theater business was back.
Then, bankable blockbuster franchises like Pixar’s Toy Story spinoff “Lightyear,” the Harry Potter film, “Fantastic Beasts: Secrets of Dumbledore” and Marvel’s new superhero, “Morbius,” all underperformed at the box office casting doubt on the post-Covid renaissance of the in-theater experience.
Now, it’s rare that I get to compare the telemedicine industry to a Spiderman movie, but the comparison here is not as much of a non-sequitur as you might think. In the early days of Covid, utilization of telemed services grew faster than streaming video subscriptions to Netflix, Apple TV and Disney+.
In fact, the telemedicine industry’s expansion from less than one percent of office visits, pre-pandemic, to a high of 16 percent of visits by mid-April 2020 spawned massive interest and investment in the telemed business model.
As the impact of Covid wanes, and consumer confidence improves, many people are questioning, and rightfully so, how much of telemedicine will persist in a post-pandemic world?
To continue the analogy, should the future of healthcare look more like Netflix (telemedicine) or AMC (in-person care)? I believe we need them both.
This month, Bicycle Health plans to roll out our virtual medication assisted treatment (MAT) care model for people with opioid use disorder (OUD) in the state of Massachusetts at the same time that we’ve stopped adding new patients in Alabama.
Where Massachusetts has taken a thoughtful, patient-first approach to improve patient access to care that includes in-person treatment and telemedicine, Alabama has made regulatory changes that make it impossible for us to operate a telemedicine within the state under our current model.
Why are we halting our service offerings in Alabama as we continue to expand to new states?
The health and well-being of our patients is our highest priority. Since we started the company in 2020, we’ve intentionally rolled our services out to patients across the country on a state-by-state basis – making sure our providers had state licenses and working within legislative parameters to do that.
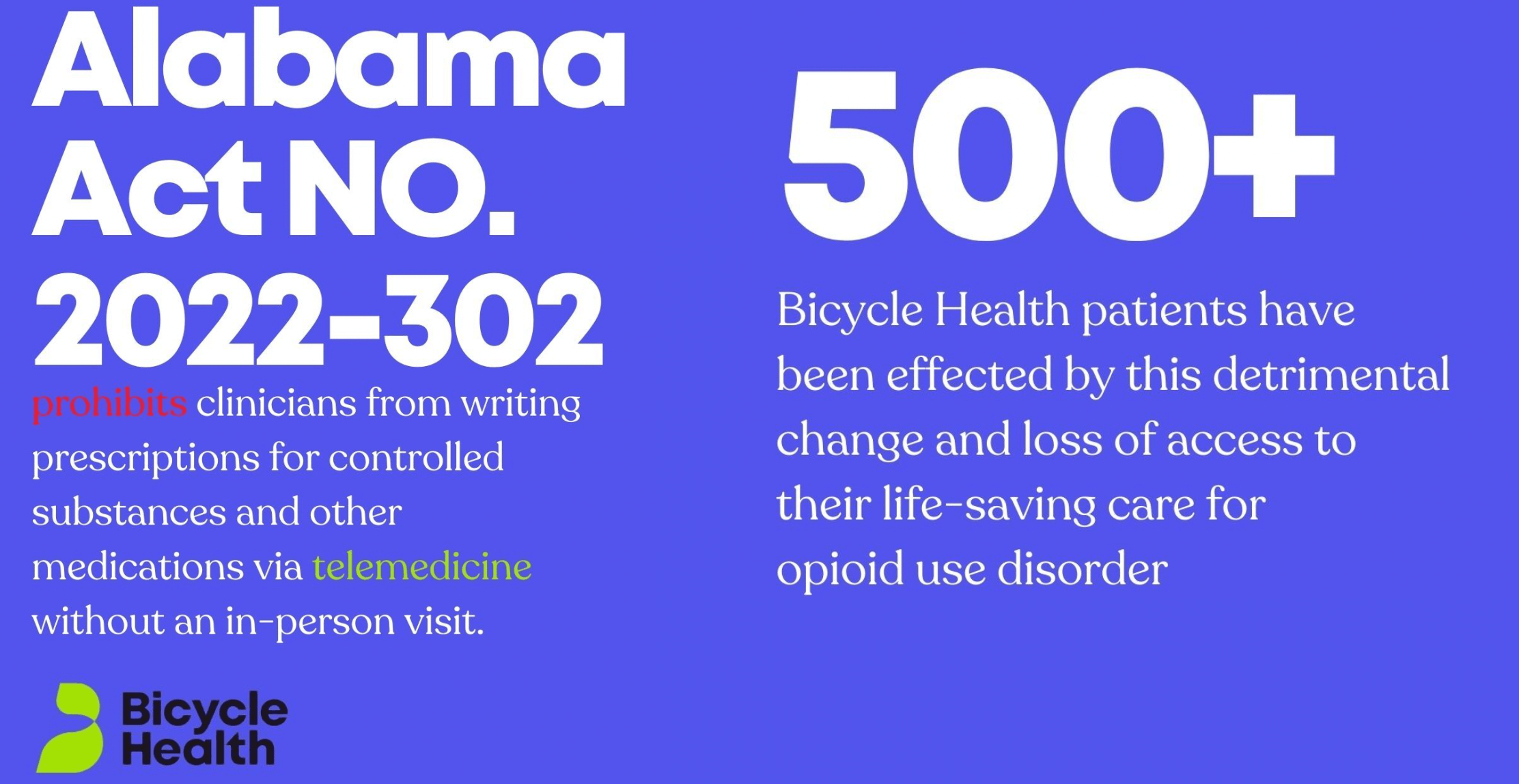
In April, the state of Alabama passed legislation requiring doctors who prescribe certain controlled medications to have at least one in-person visit with a patient each year, before continuing their care via telemedicine.
For us, it’s the equivalent of saying that Alabaman’s can only subscribe to Netflix if every movie Netflix has on its platform had at least one scene from inside the state.
Needless to say, if there were an abundance of doctors in the state who were able to see patients in-person, we would not be seeing hundreds of patients virtually in Alabama. But, we are seeing hundreds of patients in Alabama, because we know – from data, from health plans, and from patients themselves – that the lack of in-state providers has impacted people’s ability to access care. For hundreds of Alabama residents, our virtual treatment model was bridging the gap.
For all these reasons, I’m very sad to report that in order to be compliant with state regulations, we’ve made the difficult decision to stop adding new patients in Alabama.
Since the legislation passed, our team has also been working to find state-based providers who can take over treatment for our patients. We have patients as far north as Huntsville and as far south as Mobile, and everywhere in-between, which has made finding them in-state options a challenge.
Reasons for Optimism
The good news is most states are working hard to expand access to quality care through telemedicine providers. In fact, much of the Alabama law that has caused us to pause service in the state was written with the same intent.
It’s our hope that as we continue to work through the American Telemedicine Association, we may once again be able to care for patients in that state. In the interim, we’re committed to working with our partners in the state to find a long-term solution for our patients.
Telemed’s Future
As we evaluate where healthcare goes post-COVID, we might see more shifts – both toward and away from virtual care. After all, in-person visits can and should rebound for the types of care that require a physical examination or physical treatment. Medical visits where patients need and want in-person engagement with a doctor will return. Many already have.
Where we should not expect the pendulum to swing back is in the area of mental healthcare. Why? Because most of the diagnoses in this area of medicine have never required a physical exam and provider availability (especially in specialized areas of care like addiction medicine) is already limited, before you add geography as a qualifier.
Where does in-person behavioral healthcare fail insurers, providers and patients?
Behavioral healthcare has long been a bugaboo for insurers who are regularly persecuted for the lack of mental parity in their provider networks.
Providers who want to specialize in certain areas of mental healthcare, like ADHD or opioid addiction, have an extremely hard-time filling out a panel of patients –- especially when they’re forced to recruit those patients within a geographic footprint of 40 to 50 miles.
For patients, the struggle to find any available doctors, much less one who specializes in the types of care they need, is well documented. But, for those who do find care, getting regular time off work often requires disclosing uncomfortable PHI to their employer.
Telemedicine solved all of these problems during Covid, overcoming concerns about efficacy. Since then, we’ve clinically validated the efficacy of our model in addition to increasing access to critical care, decreasing costs for payers and building patient panels for specialists. In examining the pitfalls of in-person care, it’s clear that we cannot afford to lose the virtual care movement ushered in by the COVID-19 pandemic – for the sake of insurers, doctors, and, most importantly, patients.
+++
Postscript – We’re disappointed to have to pause care in the state of Alabama – especially when we see a clear need. In 2020, the Alabama Department of Mental Health reported that opioid overdoses increased more than 20%, resulting in the state being one of 25 with the highest increase during the time period. These data points alone reflect a high need for accessible treatment options that transcend in-person care.
At the same time, we’re thrilled to be entering the state of Massachusetts which has thoroughly studied the issue of medication assisted treatment (MAT) for opioid use disorder (OUD) and understands the impact it can have on public health.
A 2019 analysis from MassHealth (1) on the impact of MAT found the following results:
- “OUD patients account for ~5.5% of all MassHealth managed care eligible members.
- Spending on patients with OUD represents $1.5B (9%) of the $17.2B overall MassHealth spend in 2017″
- Members on MAT had “significantly lower costs for acute care including inpatient hospitalizations and emergency rooms contributing to a 15% reduction healthcare costs in 2017”
- The more a member was adherent to MAT, the more hospitalizations and emergency rooms decreased; adherence reduced costs by 18%
We know we have our work cut out for us as scrutiny for telemedicine in the behavioral health space rises, but this kind of research gives me hope. Especially when we know our model significantly improves adherence to MAT for people with OUD (2)
As we continue to bring life-saving care to new states and engage new patients, we have faith in our care model, in our clinical community, and in the recovery journey itself. We might have lost this battle (for now), but I think we’ll win the war.

By Ankit Gupta
Ankit Gupta, MS, is the Founder and CEO of Bicycle Health. He is passionate about the power of technology to create patient-centered experiences that can deliver high quality outcomes at ... Read More
- MassHealth: Assisted Treatment Analysis; MAT Commission Presentation; Peg Harvey & Adam Stoler, May 21, 2019 (https://www.mass.gov/doc/masshealth-presentation-on-mat-initiation-among-members-with-opioid-use-disorder/download)
- https://www.bicyclehealth.com/research
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.
