Suboxone is a safe and effective medication doctors use to treat opioid use disorder (OUD). Like most medications, Suboxone can cause side effects. Understanding what they are can help you know what to expect when you start this important sobriety treatment.
What Is Suboxone Used For?
Suboxone is a prescription medication. The U.S. Food and Drug Administration (FDA) approved it to treat opioid dependence.[1]
Suboxone contains the following two active ingredients:[1]
- Buprenorphine, a partial opioid agonist, to ease opioid withdrawal symptoms and cravings
- Naloxone, a misuse deterrent, is activated only when people take too much or tamper with their doses
The FDA says Suboxone works best when provided alongside other OUD treatments.[1] Counseling, education and therapy can help people build up sobriety skills, while Suboxone eases relapse risks.
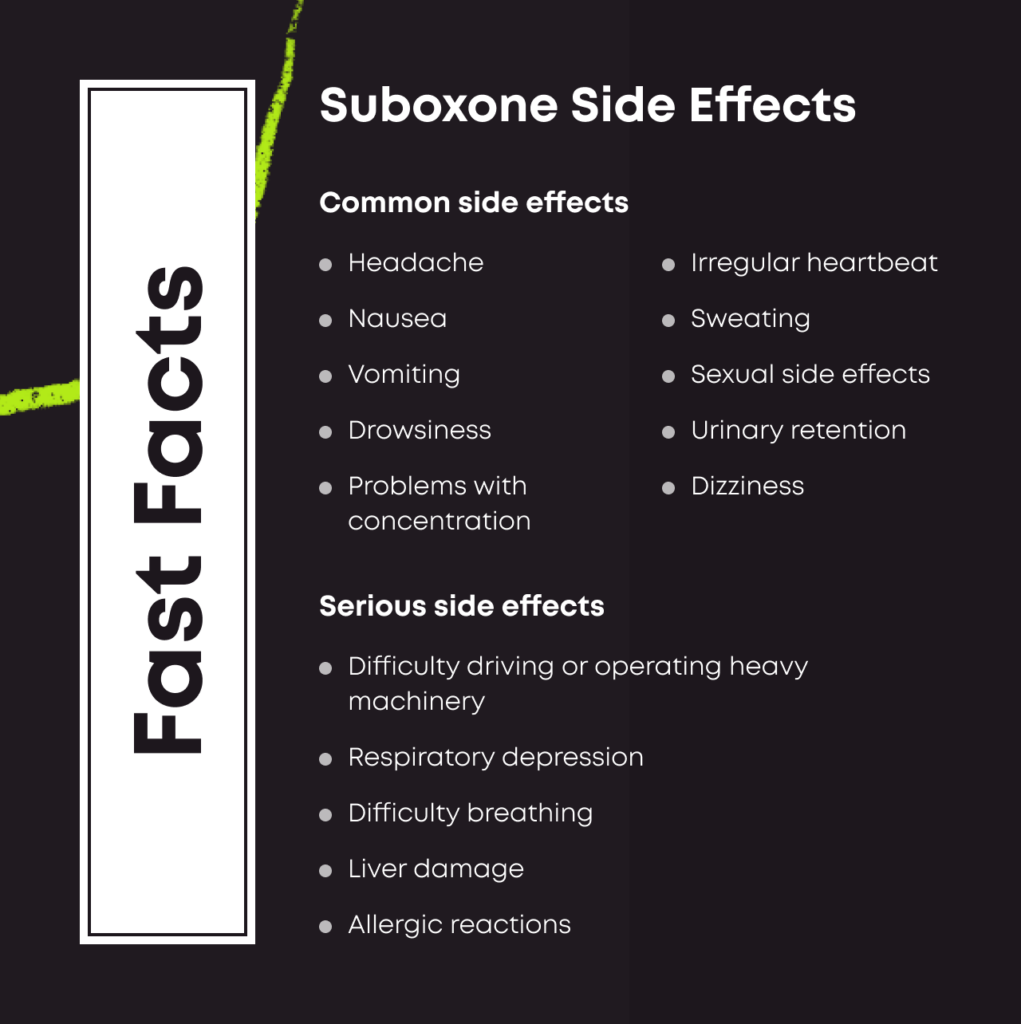
Understanding the Different Side Effects of Suboxone
Suboxone’s side effects vary from mild and common to severe and rare. Your doctor should explain these symptoms to you before your treatment begins. Here’s what you should know:
Common Side Effects
The FDA says the following side effects are often seen in people using Suboxone:[1]
- Numbness of the tongue, cheek, lips, or gums
- Burning sensation in the mouth
- Sores inside the mouth
- Headaches
- Nausea
- Vomiting
- Excessive sweating
- Constipation
- Insomnia
- Pain
- Swelling in the hands and feet
Serious Side Effects
While Suboxone is a safe and effective medication, it can cause severe and unusual reactions in some people. The FDA says the following side effects have been reported in people taking Suboxone:[1]
- Life-threatening respiratory depression
- Adrenal gland insufficiency
- Liver damage
- Allergic reactions, including rashes, hives, and swelling
- High blood pressure
Contact your doctor immediately if any of these side effects occur.
Precipitated Withdrawal
Suboxone is designed to block opioids. Take it too early, and it could kick active drugs off their receptors. Intense withdrawal symptoms can begin, such as nausea, vomiting, muscle aches and anxiety.
Your risk of precipitated withdrawal is higher depending on a few factors:[2]
- Your dose: The more Suboxone you take, the greater the risk of causing withdrawal if there are still opioids in your system.
- Your dosing interval: The biggest cause of precipitated withdrawal is taking a first dose of Suboxone too soon after taking full opioids. Usually, doctors recommend waiting at least 12 to 24 hours after your last opioid dose or until you feel natural withdrawal symptoms before taking your first dose of Suboxone.
- Your history: The more dependent you are on opioids, the greater your risk of withdrawing if opioids are stopped too quickly.
Following your doctor’s instructions carefully before taking your first dose of Suboxone is the best way to avoid precipitated withdrawal.
Factors That Determine the Severity of Suboxone’s Side Effects
Anyone can develop side effects due to their prescription use, but some factors could raise your risk.
You’re more likely to experience Suboxone side effects due to the following:[1]
- Underlying health issues: You may have more side effects from Suboxone if you have other co-occurring health conditions.
- Suboxone dose: Larger doses can cause more side effects.
- Misuse: Shooting, snorting, or otherwise tampering with your Suboxone can lead to more side effects.
- Combining medications: Taking Suboxone with other medications increases your risk of side effects.
Tips to Help Prevent Negative or Severe Side Effects
You’re not required to endure side effects from Suboxone doses. Taking a few basic steps can help to reduce your risk of experiencing severe side effects.
The following tips can help:[1]
- Take your medications as directed. Don’t take Suboxone in any way other than exactly as prescribed. Take them on the schedule your doctor recommends.
- Identify your other medications. Suboxone can interact with many other substances, including benzodiazepines. Tell your doctor about every other drug you’re using.
- Check in with your doctor. Routine checkups can help your doctor look for problems like liver issues.
Understanding Suboxone Withdrawal
If you stop Suboxone treatment cold turkey, you can experience withdrawal symptoms. The buprenorphine component inside your medication is an opioid. Quit too quickly, and your brain cells can overreact with physical and mental symptoms.
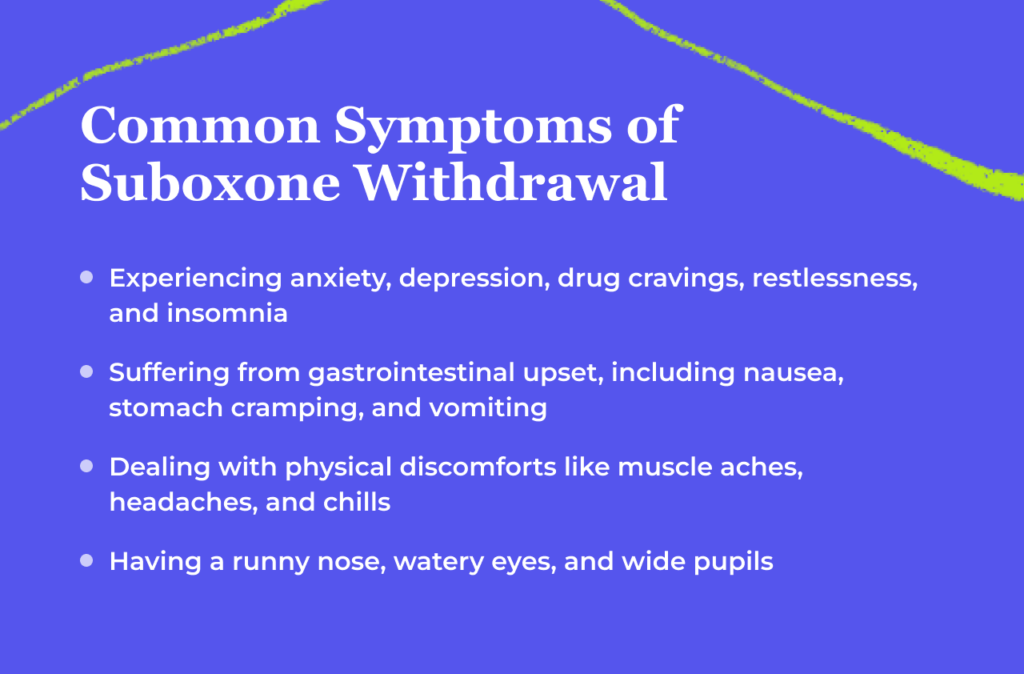
Common Suboxone Withdrawal Symptoms
Opioid withdrawal symptoms are often described as flu-like. They can include the following:[3]
- Agitation
- Anxiety
- Aching muscles
- Watery eyes
- Insomnia
- Runny nose
- Sweating
- Diarrhea
- Nausea
- Vomiting
Withdrawal Timeline
Suboxone withdrawal can last between 10 and 20 days.[4] How long your issues last depends on factors like your health, dependence on opioids, and personal addiction history.[2,3]
| Time Frame | Symptoms |
| 8–24 hours | Early symptoms like agitation, anxiety, aching muscles, and insomnia begin. |
| 4–10 days | Late symptoms like nausea, abdominal cramping, diarrhea, and vomiting start. |
| Day 11 onward | Symptoms begin to fade. But cravings and poor mental health can persist. |
Frequently Asked Questions About Suboxone Side Effects
We’ve compiled some of the most frequently asked questions about Suboxone side effects.
Common side effects associated with Suboxone include headaches, nausea, vomiting, excessive sweating, constipation, insomnia, pain, and swelling in the hands and feet.
Sexual problems aren’t listed as side effects in documents produced by the FDA.[1] But opioids are known to cause at least some sexual side effects.
Yes. Side effects can vary from one person to another.
Precipitated withdrawal is the sudden onset of drug withdrawal caused by the too-early use of opioid blockers. Suboxone can cause this problem, but your doctor will work hard to ensure you don’t take your first dose before it’s safe to do so.
Never skip a Suboxone dose without asking your doctor first. It’s not safe to skip doses without consulting with a professional.
Anxiety is a known side effect of Suboxone. But recovery from the use of opioid drugs like heroin can cause anxiety too. If you experience this symptom, talk to your doctor about what to do next.

Reviewed By Peter Manza, PhD
Peter Manza, PhD received his BA in Psychology and Biology from the University of Rochester and his PhD in Integrative Neuroscience at Stony Brook University. He is currently working as a research scientist in Washington, DC. His research focuses on the role ... Read More
- Suboxone prescribing information. U.S. Food and Drug Administration. Published March 2021. Accessed October 12, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/022410s042lbl.pdf
- Rosado J, Walsh SL, Bigelow GE, Strain EC. Sublingual buprenorphine/naloxone precipitated withdrawal in subjects maintained on 100mg of daily methadone. Drug Alcohol Depend. 2007;90(2-3):261-269. https://doi.org/10.1016/j.drugalcdep.2007.04.006
- Opiate and opioid withdrawal. U.S. National Library of Medicine. Published April 30, 2022. Accessed October 12, 2023. https://medlineplus.gov/ency/article/000949.htm
- Withdrawal management. Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Settings. Published 2009. Accessed October 12, 2023. https://www.ncbi.nlm.nih.gov/books/NBK310652/
Download Our Free Program Guide
Learn about our program, its effectiveness and what to expect
Imagine what’s possible on the other side of opioid use disorder.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.
